A guide to beating inflammation and managing chronic pain
What do heart disease, arthritis, cancer, diabetes, Alzheimer’s disease, chronic fatigue, and persistent pain all have in common? Inflammation. So, what is inflammation? How does inflammation cause pain, and can food and nutrition really help?
What is Inflammation?
The word inflammation comes from the Latin word ‘inflammare’, to ‘set on fire’. You’re probably familiar with the concept of acute inflammation, for example, if you bump your knee or scrape your elbow. The immune system revs up and white blood cells rush to the scene. The area swells, and fluid immobilizes the area while the body takes care of the problem. You experience the symptoms of pain; heat, redness, and swelling, otherwise known as acute inflammation. The onset is fast, usually within minutes or hours, and the signs are prominent, for instance, you may see a lump or a cut. As your body heals, the inflammation subsides, and the redness and swelling disappear.
Inflammation is not inherently bad. In fact, it is necessary in order to heal wounds and fight off pathogens. The inflammatory process is normally controlled and self-limited. That said, there is another kind of inflammation we experience called chronic inflammation. This low-grade condition can persist for long periods of time in your body, and if left unchecked, can become the source of great discomfort.
Chronic Inflammation Adds to Pain
Chronic, or systemic inflammation, as it is sometimes called, differs from acute inflammation in that you cannot treat it with a bag of ice or an ace bandage. The signs of chronic inflammation are less prominent than those of acute inflammation, making it harder to pinpoint the cause of pain, and the onset is much slower; taking place over days and sometimes months.
Chronic inflammation is the source of many of the diseases we currently treat. This low-level inflammation contributes to the pathogenesis of the most fatal diseases in the United States, including heart disease, cancer, chronic respiratory disease, stroke, Alzheimer’s disease, diabetes, and nephritis. (1) Autoimmune diseases have their roots in chronic inflammation, and once triggered, they can linger undetected for years, even decades. Today, 50 million Americans live with an autoimmune condition, while many more are developing inflammation that can lead to autoimmunity. Inflammatory conditions also carry with them the added complications of pain, fatigue, and anxiety.
How To Test for Inflammation?
If systemic inflammation goes undetected, how do you even know if you suffer from the condition? One of the best ways to measure the level of inflammation in your body is by checking high-sensitivity C-reactive protein (hs-CRP) levels. C-reactive protein is made in the liver, and it helps to protect your body and fight off infections. Your hs-CRP lab report doesn’t tell you exactly what is causing the inflammation, but it gives you an idea of how much inflammation you have in your body. High levels of CRP are often found in conditions such as the following:
-
- Rheumatoid arthritis
-
- Metabolic Syndrome
-
- Chronic Fatigue
-
- Cancer
-
- Heart disease
-
- High blood pressure
-
- Infections
The hs-CRP test is fairly inexpensive. Another reasonably priced test is fibrinogen. If you want to delve deeper into testing inflammatory markers, a few more costly labs are: tumor necrosis factor-alpha (TNF-alpha), interleukin-1 beta (IL-beta), interleukin-6 (IL-6), and interleukin-8 (IL-8). (1)
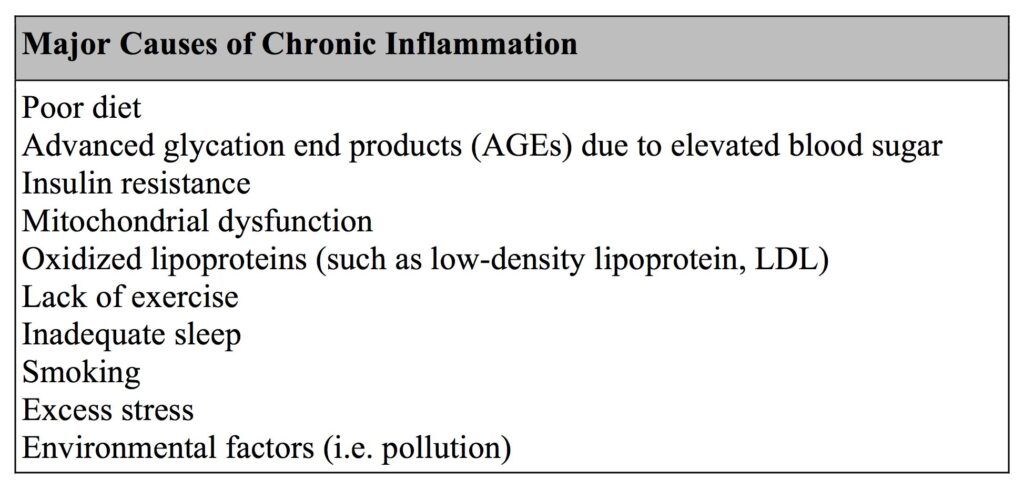
What Causes Chronic Inflammation?
Many chronic inflammatory conditions originate from an unhealthy diet and lifestyle. Those who consume the Standard American Diet (SAD) are more prone to elevations of blood sugar and hbA1c, and also to higher levels of low-density lipoproteins (LDL), also known as the “bad cholesterol.” These can all lead to systemic inflammation. If blood sugar is consistently high, the circulating sugars (mostly glucose and fructose) come into contact with proteins and lipids in your system and create damaging compounds called advanced glycation end products (AGEs). These molecules bind to receptors called RAGEs, or “Receptors for Advanced Glycation End Products”. The RAGE complexes trigger the activation of nuclear factor kappa-B (NFkB), which then activates numerous inflammatory genes. AGEs originate in elevated blood glucose levels, however, they can also come from foods that are cooked at high temperatures, especially red meat. (2)
High insulin levels are also inflammatory and are often a hallmark of chronic disease. Insulin resistance can develop by eating too many refined carbohydrates which are rapidly converted into fat, triggering an inflammatory cascade. For this reason, the goal is to keep blood sugar stable and to avoid large spikes that cause an increase in insulin.
Mitochondria are the cellular organelles responsible for generating energy. Dysfunction in mitochondrial function can occur from toxins in our food or environment, smoking, reactive oxygen species, and aging. As a byproduct, mitochondria produce free radicals. These molecules can initiate a flood of inflammatory signals resulting in cell death. With a decline in mitochondrial efficiency and an increase in free radical production, chronic inflammation can occur. (3)
Other lifestyle factors such as smoking, lack of exercise, inadequate sleep and stress can cause inflammation. Disruption of normal sleep can lead to daytime elevations of pro-inflammatory molecules. A study in the Journal of Clinical Endocrinology and Metabolism found that plasma levels of TNF-alpha and IL-6 were elevated in patients with excessive daytime sleepiness, including those with sleep apnea and narcolepsy (4) Both physical and emotional stress can lead to the release of inflammatory cytokines such as IL-6. Stress is also associated with decreased sleep and increased body mass, due to the release of the stress hormone cortisol. (5) Chronic stress increases glucocorticoid receptor resistance, which results in a failure to downregulate the inflammatory response.(6) Some factors are beyond our control, but there are numerous lifestyle changes we can make to prevent and reverse the chronic inflammation that leads to pain.
 The Inflammation-Pain Connection
The Inflammation-Pain Connection
Those with chronic inflammation often suffer from pain, fatigue, anxiety and mood disorders. In a study of European patients with advanced cancer, an increase in the inflammatory marker hs-CRP was associated with greater pain and fatigue.(7) Research shows that pro-inflammatory cytokines may have a direct action on pain via sensory neurons or an indirect action by way of other inflammatory mediators called prostaglandins.(8) In another study, patients with Rheumatoid Arthritis had higher levels of pro-inflammatory IL-1 in their cerebrospinal fluid, which was associated with greater fatigue, pain and mood issues. (8) More recently, an investigation in chronic inflammation demonstrated the connection between elevated levels of the pro-inflammatory cytokines, IL-1, IL-6, IL-8, TNF-alpha and increased pain. (9)
Food is An Inflammation Fighter
There are many ways to conventionally treat and manage pain, such as pharmaceutical medications and nerve blocks. Effective as they cam be, these are not long-term solutions. One of the most exciting ways to manage chronic pain is by adopting an anti-inflammatory diet. This natural approach can often eliminate the unpleasant side effects of medications that cause sleepiness, a foggy brain, and memory loss. Dr. Welches, DO, of the Cleveland Clinic states, “Following an anti-inflammatory diet is a powerful therapy for pain control with many beneficial side effects. The anti-inflammatory diet is considered an integrative approach to pain management, along with exercise, stress management, osteopathic manipulation therapy and acupuncture.” (10)
Research shows that an anti-inflammatory diet can ease fibromyalgia and chronic pain symptoms. A recent study in rodents found that exposure to a high energy diet (high sugar and fat), similar to the Standard American Diet, resulted in changes to their neuronal signaling pathways that alter nociceptive responses to pain. This means that the animals eating the SAD diet were less tolerant to pain than those that were fed a healthier diet. (11)
SAD (Standard American Diet) and Systemic Inflammation
Can the type of food you eat truly affect your sensitivity to pain? In a rodent study, it was shown that the Standard American Diet (SAD) leads to an increase in fat mass, with a decrease in lean mass. Significant increases in serum leptin (a satiety molecule released from adipose tissue) and pro-inflammatory cytokines such as IL-6 and TNF-alpha) were evident, as well as a greater than 2-fold increase in circulating monocytes and neutrophils. This systemic inflammation resulted in a hypersensitivity to pain. In these animals, prolonged exposure to a poor diet led to altered nociceptive sensitivity, along with chronic inflammation and persistent pain. In a nutshell, a poor diet can lead to the activation of the immune system, which releases pro-inflammatory cytokines that elicit pain. (12)
Chronic inflammation and pain can actually occur just from being overweight. In one human study, of those reporting chronic pain, 58% were overweight or obese, indicating that more chronic pain sufferers are above normal weight than not. (13) However, diet itself can cause the chronic elevation of inflammatory cytokines, which can result in prolonged hypersensitivity to pain. This is an important finding, for the reason that people who consume the SAD diet containing a high percentage of carbohydrates and unhealthy fats, may experience chronic inflammation even in the absence of obesity. So, it is important to consider that the quality of one’s diet can affect inflammation and pain independent of weight. (12)
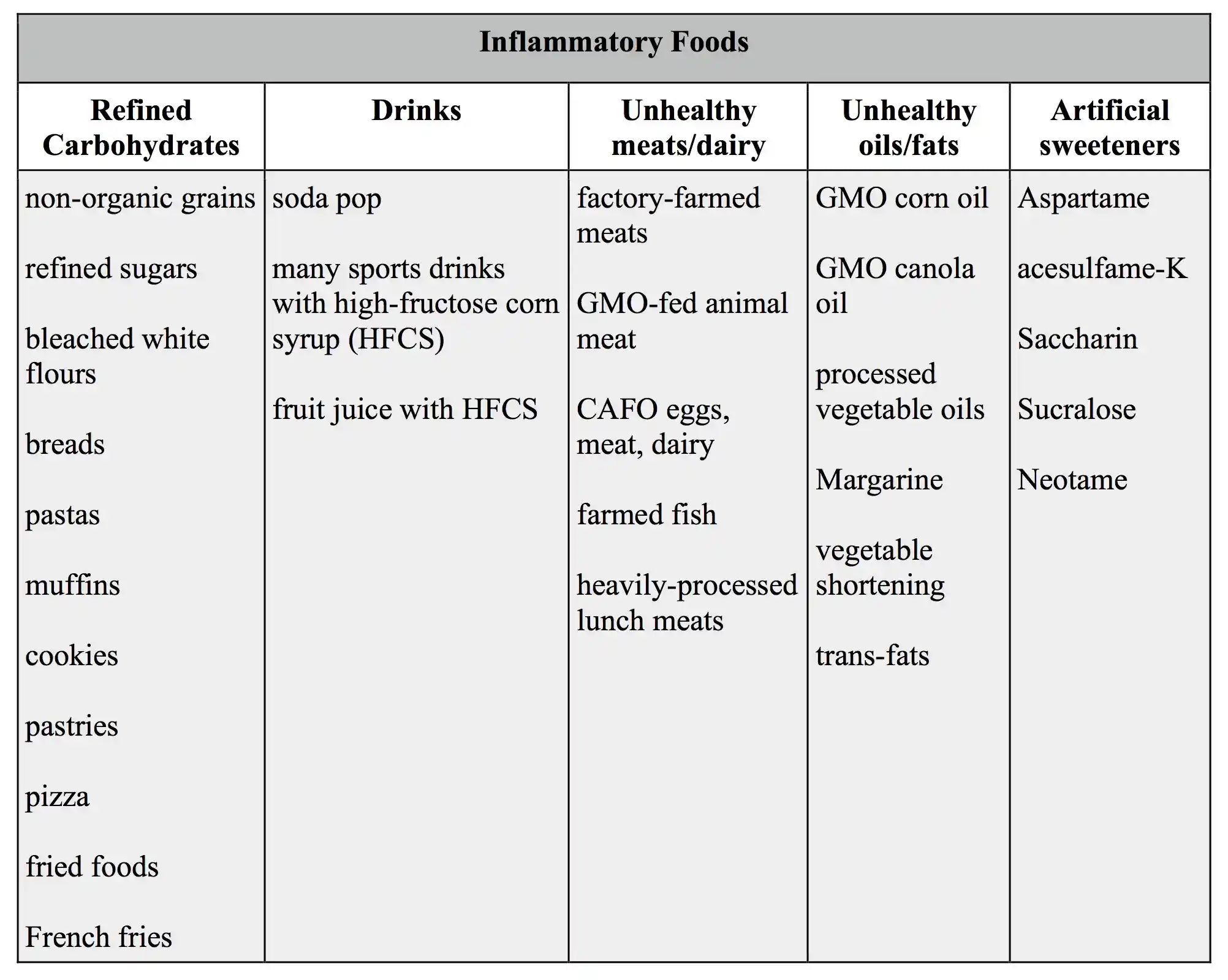
What kinds of foods should one avoid in order to reduce the inflammation that may cause pain? You’ll want to limit added sugars, avoid highly-processed grain products, reduce dairy (if you choose dairy, make sure it’s organic and from a clean source), be careful with your fats (stay away from processed vegetable oils and trans-fats that are found in many packaged snacks), and look for products without additives, artificial sweeteners or colorings. To the best of your ability, avoid genetically-modified (GMO) and non-organic foods, as well.
Avoid these foods to reduce inflammation and alleviate pain:
Click here to learn how to use nutrition to treat chronic pain!
Anti-inflammatory Meals are Medicine
Let’s turn off the pro-inflammatory cytokine ‘switch’ to reduce inflammation and relieve pain. The path to healing begins at the end of your fork, and the ingredients are right in your kitchen!
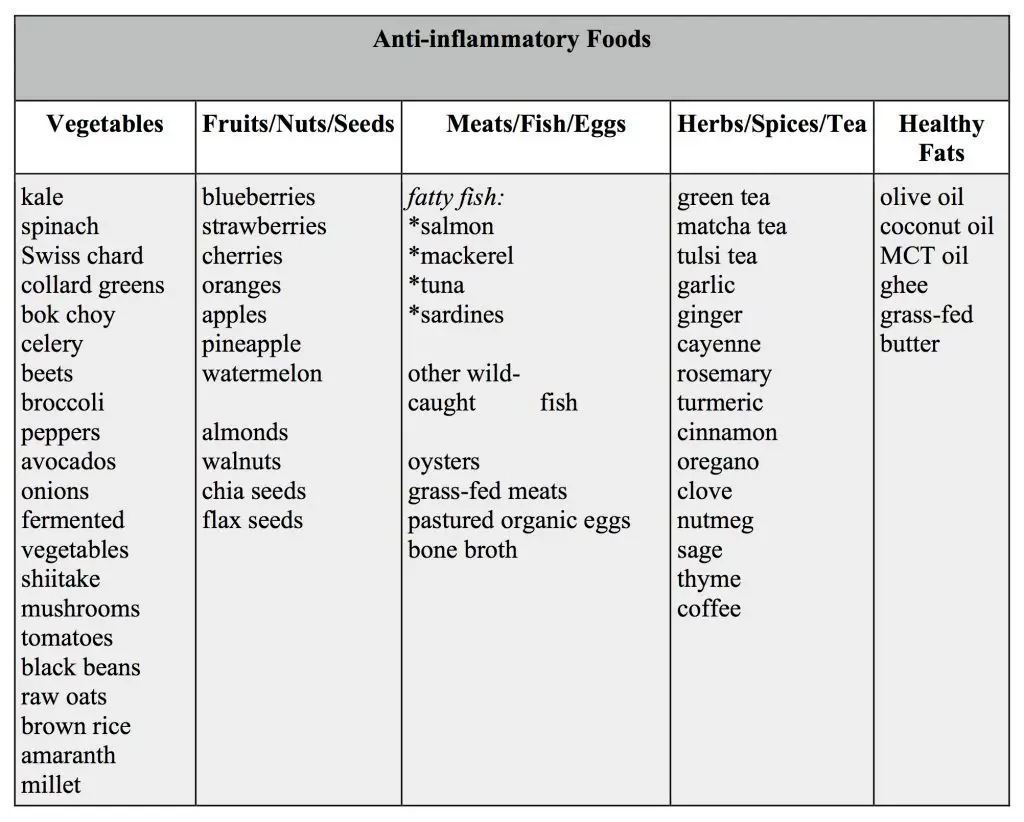
Here are the basic tenets of an Anti-inflammatory Diet:
- Consume whole foods, and eliminate processed junk
- Strive to buy clean foods: organic, non-GMO, grass-fed, wild-caught
- Reduce the amount of carbohydrates, especially processed carbs
- Include healthy, clean sources of protein
- Good fats are important, especially the omega-3 fatty acids
- Add a wide variety of vegetables and fruits to your meals
You can’t go wrong when you choose whole foods. Since they don’t have nutrition labels with a long list of ingredients, you don’t have to worry about additives, preservatives and excess commercial processing. If you ditch the packaged foods, you’ve won half the battle. Choose clean meats and fish to bake or grill, and fresh veggies to eat cooked or raw. Instead of commercial snacks, enjoy fresh fruit, nuts, and organic cheeses or plain yogurt (in moderation).
Buy clean-sourced foods when possible. Genetically-modified (GMO) and non-organic products contain more pesticides and herbicides. These chemicals can be toxic to the nervous system thus can result in exacerbated pain. They can also disrupt hormone pathways, leading to weight gain. Look for the USDA organic label for better quality foods. Farm animals that are grass-fed, pastured, cage-free or wild-caught are more humanely treated, and healthier than CAFO animals (concentrated animal feeding operations). They contain no added hormones or antibiotics and many are fed organic feed. Non-GMO vegetables and fruits raised organically have lower chemical residues.
An overabundance of carbohydrates, especially processed ones, can lead to blood sugar dysregulation and insulin resistance. Healthy carbs come from fresh vegetables and fruits, nuts and seeds, legumes and healthy whole grains like wild rice, quinoa, and raw oats. These foods also contain lots of fiber, which sadly, is lacking in the SAD diet. Getting enough fiber will help battle inflammation.
Fat has gotten a bad rap over the last 50 years, primarily because of cardiovascular disease, but not all fat is bad. Eating too much saturated fat (animal fat) and omega-6 fat (corn oil, soybean oil, vegetable oil) can be pro-inflammatory. But adding fats high in omega-3 can have potent anti-inflammatory effects. (6) Healthy fats can be found in fish, nuts, seeds, eggs, and certain oils, such as walnut, flaxseed, avocado, olive, and coconut.
Make half your plate vegetables and fruits, and as they say, “eat the rainbow”! The anti-inflammatory diet is full of color, which provides an array of healing phytonutrients. Decorate your plate each day with nature’s colors. Red apples, tomatoes, and radishes. Orange carrots and mangoes. Yellow pineapple and summer squash. Green peppers, asparagus, and arugula. Blue and purple berries, plums, grapes, eggplant, and potatoes. White cauliflower, coconut, onions, and mushrooms. Adopting an anti-inflammatory diet can be nutritious, delicious and fun!
Add these anti-inflammatory foods to help ease your pain:
Dynamite Dietary Nutrients
Below are just some of the powerful components that are intrinsically part of a healthy anti-inflammatory diet:
Omega-3s
Many of us don’t receive adequate amounts of omega-3 fatty acids in our diet. Omega-3s are good fats which can be found in cold water fish, like salmon, tuna, mackerel and herring, and also in walnuts and avocados. These fats protect the body by inhibiting prostaglandins, molecules that trigger inflammation. A higher intake of omega-3 fatty acids is associated with lower levels of CRP, TNF-alpha, and IL-6. It also increase central serotonergic activity which alleviates pain. Omega-3 supplementation has been effective for migraines, low back and joint pain, Rheumatoid Arthritis, and other autoimmune conditions.
Sulphoraphane
 Vegetables such as broccoli, cauliflower, kale, Brussels sprouts and some other green leafy vegetables contain a chemical called sulphoraphane, which can reduce inflammation and block enzymes that can cause joint deterioration and pain. It may also be able to improve the linings of blood vessels due to chronic blood sugar problems and persistent inflammation. (14)
Vegetables such as broccoli, cauliflower, kale, Brussels sprouts and some other green leafy vegetables contain a chemical called sulphoraphane, which can reduce inflammation and block enzymes that can cause joint deterioration and pain. It may also be able to improve the linings of blood vessels due to chronic blood sugar problems and persistent inflammation. (14)
Anthocyanins
Berries (cherries, blueberries, raspberries, strawberries) pack a punch when it comes to anti-inflammatory substances. They contain polyphenol compounds, particularly anthocyanins, which can lower CRP levels and inflammation. The Arthritis Foundation reports that some investigators compare the properties of tart cherries to the effects of NSAIDs (nonsteroidal anti-inflammatory drugs). (15) Reduce inflammation and pain the delicious way, by having a cup of berries every day.
Magnesium
Studies have shown that magnesium can help reduce serum C-reactive protein levels, inhibiting inflammation. (16) (17) Magnesium is required for hundreds of biochemical reactions in the body, yet studies report that 20 to 40 percent of people are deficient of this important mineral. Magnesium is helpful for those suffering from migraine headaches as well as fibromyalgia. Foods high in magnesium are dark green leafy vegetables, nuts and seeds, whole grains, avocados, bananas, dried fruit, fish, yogurt and yes, dark chocolate!
EGCG
 Enjoyed for centuries, the daily consumption of tea is second only to water, and it has been associated with numerous healing properties. Among the many benefits of green tea is its ability to reduce a substance called HMGB1 (high mobility group box-1) which is a molecule that triggers the release of inflammatory cytokines. The EGCG (epigallocatechin-3-gallate) substance in green tea has been shown to attenuate both HMGB1 and IL-6. (18) Enjoy a cup or two a day, while you ease your inflammation and pain.
Enjoyed for centuries, the daily consumption of tea is second only to water, and it has been associated with numerous healing properties. Among the many benefits of green tea is its ability to reduce a substance called HMGB1 (high mobility group box-1) which is a molecule that triggers the release of inflammatory cytokines. The EGCG (epigallocatechin-3-gallate) substance in green tea has been shown to attenuate both HMGB1 and IL-6. (18) Enjoy a cup or two a day, while you ease your inflammation and pain.
Micronutrients in Spices
Add a little spice to your life by experimenting with various herbs and spices. Many spices possess anti-inflammatory compounds that inhibit the biochemical processes of inflammation. Curcumin, one of the compounds in turmeric has been studied in over 7000 published scientific articles and is known to modulate numerous inflammatory pathways. Give your taste buds a treat by incorporating ginger, turmeric, rosemary, oregano, cayenne, cloves and nutmeg into your daily meals. A tasty way to reduce inflammation.
Lifestyle factors that can reduce inflammation and pain
In addition to adopting an anti-inflammatory diet, you can try these lifestyle tips that are known to lower inflammation:
-
- Eat according to your natural circadian rhythm. Research shows that eating earlier in the day, and refraining from late night eating can help stabilize weight, which in turn, will keep inflammation under control.
-
- Keep a healthy weight. Managing your weight will automatically reduce inflammation and associated pain. Excess adipose tissue (fat tissue) triggers low-grade, systemic inflammation.
-
- Engage in regular exercise. Studies show that exercise can lower many cytokines and pro-inflammatory molecules independent of weight loss. When you use your muscles, they actually cause a pro-inflammatory state, but surprisingly, the overall systemic inflammation is decreased. (19) Moderate exercise for 30 minutes at least three times a week has been shown to significantly improve insulin sensitivity, reversing insulin resistance. (6) This helps bring down inflammation and pain levels.
-
- Get adequate sleep and practice good sleep hygiene. Staying up late is not good for your cortisol levels, or for weight management. Aim for 7-9 hours of sleep per night, the hours before midnight being the most beneficial. Practice good sleep hygiene by winding down earlier in the evening, turning off computer screens and electronics, and by keeping your bedroom cool, quiet and dark.
-
- Manage your stress levels. Keep your stress hormone, cortisol, in check by practicing some mindfulness each day. Meditation, prayer, journaling, walking in nature, or gentle yoga are some good examples. Choose one that fits your lifestyle.
The low-grade, systemic inflammation that eventually leads to chronic disease doesn’t happen overnight. Nor is it resolved in a day, or with a magic pill. With all health-related matters, changes in daily habits are required to maintain lasting results. However, if you take it one day at a time, and start slowly by incorporating some of the basic components of an anti-inflammatory lifestyle, you will no doubt discover how powerful the right nourishment can be for healing. Better yet, you are likely to find the new diet more delicious and more rewarding!
Click here to learn how to use nutrition to treat chronic pain!



