Can the food you eat help ease pain? Can the pain associated with chronic diseases be reduced by adopting a specific diet? Read on as we continue to explore some of the current evidence around diet and pain. This is Part 2 of a 2-part series.
[Go here for Which Diet Works for Pain? [The Evidence] Part 1]
Is the pain you are experiencing related to the food you are eating? Consuming unhealthy foods can cause your body to release molecules called cytokines, that trigger an inflammatory response. When your immune system is overloaded with these chemicals, a chronic inflammatory state may ensue, causing pain. Those with chronic illness often take medications for pain, which may wind up reducing symptoms by only 30% to 50%. Today, many patients turn to diet and lifestyle changes for additional relief. By making some simple diet changes, you can start taking control of your health as you travel on your healing journey.
During the first half of the 2-part series, we discussed the Mediterranean Diet, the Ketogenic Diet, a Plant-based Diet and Intermittent Fasting, and how they can assist in relieving some of the pain associated with chronic disease.. Here we dive into the research behind the Low-FODMAP Diet, the Paleo Diet, and the Autoimmune Protocol (AIP).
The Low-FODMAP Diet
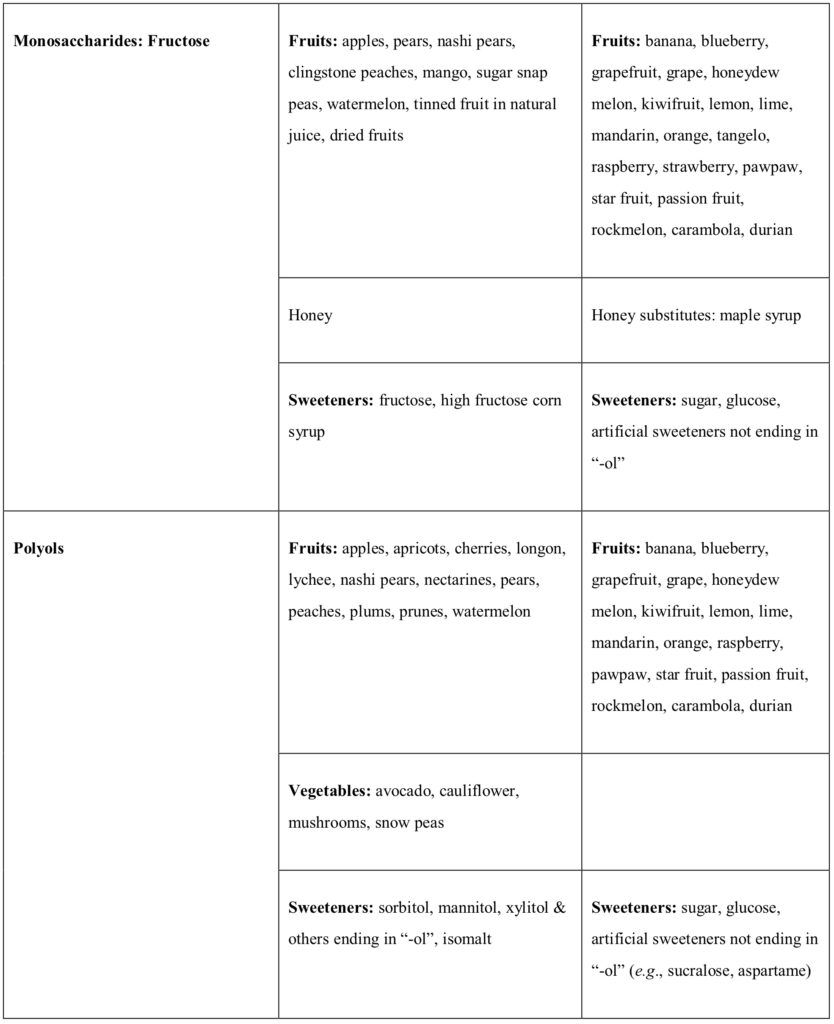
FODMAPs is an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. The term stands for a group of poorly absorbed short-chain fermentable carbohydrates that are naturally present in many foods, including garlic, wheat, legumes, dairy products, apples, and stone fruits, to name a few. FODMAPs can pass unabsorbed into the colon, where they increase water in the intestine through osmotic activity. Gas production is induced due to fermentation of these carbohydrates by colonic bacteria. This can result in abdominal distension, causing uncomfortable and painful gastrointestinal symptoms (1). The Low-FODMAP Diet removes these offending foods to relieve symptoms.

The Components of the Low-FODMAP Diet
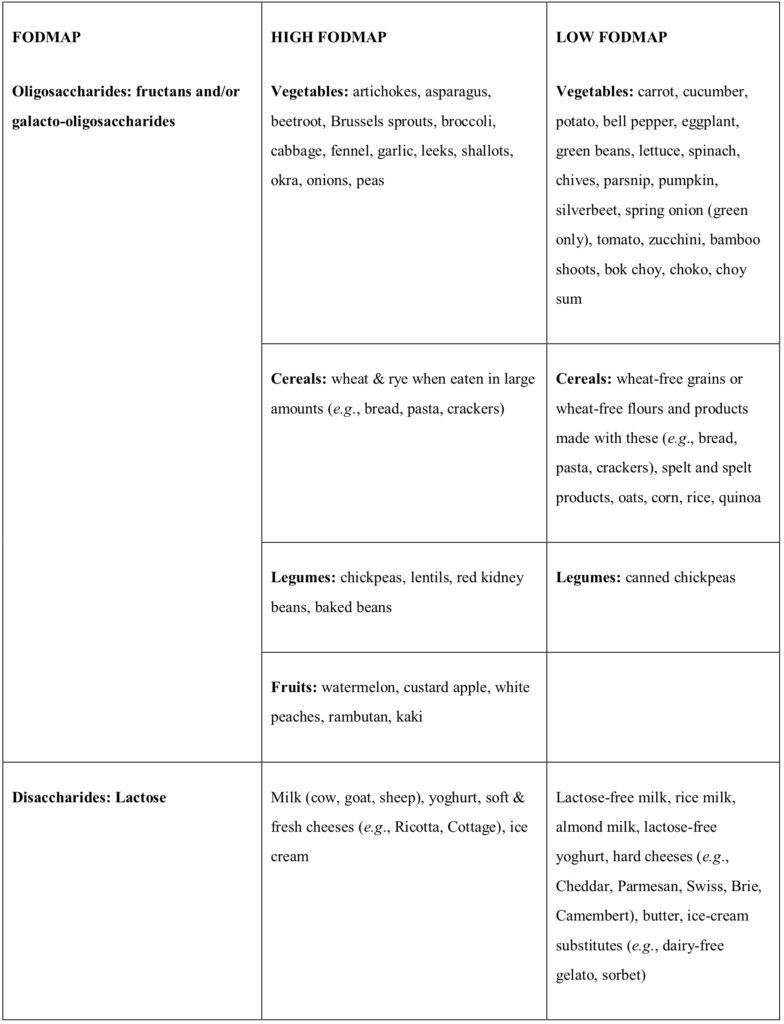
The Low-FODMAP Diet restricts the dietary intake of the fermentable carbohydrates that can lead to gastrointestinal issues. Foods are classified into “high FODMAP” and “low FODMAP” foods. See the table below for a list of high- and low-FODMAP foods (2).
High- and Low-FODMAP Foods
Benefits of the Low-FODMAP Diet
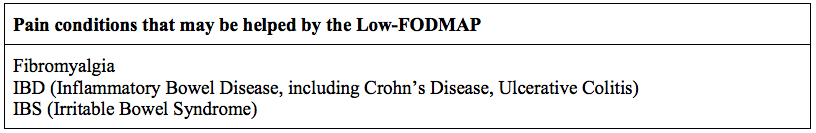
By restricting the dietary intake of High-FODMAP foods that contain the short-chain fermentable carbohydrates, the overabundance of gas production by the microbiota is reduced. Abdominal distension, caused by both the gas and additional luminal fluid is diminished, which eases pain. Marked improvement of gastrointestinal symptoms results in many patients suffering from IBD (Inflammatory Bowel Disease, which includes Crohn’s Disease and Ulcerative Colitis), Irritable Bowel Syndrome (IBS), and Fibromyalgia.
How the Low-FODMAP helps Pain
Research shows that the by-products of the interaction between FODMAPs and gut microbiota act on intestinal stem cells, resulting in abnormal differentiation of these cells into endocrine cells. This can lead to an increased number of endocrine cells in the gut. The gastrointestinal endocrine cells regulate the gut’s sensitivity, motility, secretion, absorption, local immune defense, as well as appetite (3). Therefore, disruption in the balance of GI endocrine cells may play a role in the development of visceral hypersensitivity and dysmotility (4).

Inflammatory Bowel Disease and Irritable Bowel Syndrome
There is a growing body of evidence that supports the efficacy of the Low-FODMAP diet, especially in gastrointestinal diseases including IBD and IBS. Randomized control trials (RCTs) and observational studies have demonstrated that this dietary approach can lead to an improvement in symptoms for up to two-thirds of patients with IBS (5) (6). Many IBS patients will respond to the protocol within one to four weeks of initiating the diet, as it alleviates abdominal pain, bloating, flatulence, and/or diarrhea (7) (8). In a randomized control trial, the quality of life, the level of anxiety and depression, the work productivity and sleep issues all improved in IBS-D (Irritable Bowel Syndrome with diarrhea) patients after adopting the Low-FODMAP Diet (9). A 2017 meta-analysis presented high-grade evidence of improved symptoms for IBS patients who followed a Low-FODMAP Diet compared to those on a traditional IBS diet (10). Another meta-analysis offers proof to show that a Low-FODMAP Diet helps reduce the symptoms of IBD patients, including diarrhea, abdominal bloating, abdominal pain and nausea (11).
Fibromyalgia
Fibromyalgia, a chronic, rheumatic condition characterized by widespread myofascial pain, is associated with comorbidities of gastrointestinal disorders including IBS. A 2016 study showed significant improvement in gastrointestinal symptoms as well as the pain symptoms associated with fibromyalgia in a cohort of 38 women diagnosed with the condition for an average of 10 years. Their weight, body-mass index and waist circumference decreased significantly, as did their somatic pain (12).
Implementing the Low-FODMAP Diet can be challenging for the patient. One concern is the adequate intake of fiber and calcium. In addition, restricting the consumption of prebiotic fructans and galacto-oligosaccharides may alter the intestinal microbiota (13). Dietary counseling from a nutrition professional is prudent to insure that the Low-FODMAP Diet is nutritionally sound.
Fibromyalgia, a chronic, rheumatic condition characterized by widespread myofascial pain, is associated with comorbidities of gastrointestinal disorders including IBS Share on X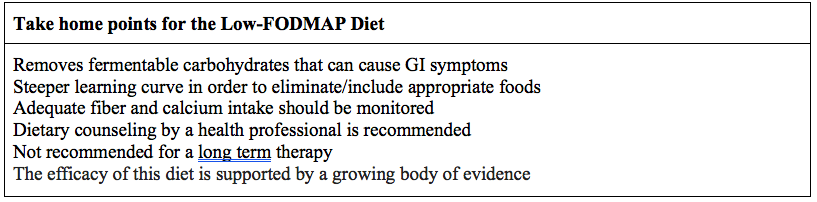
The Paleo Diet
In 1975, Dr. Walter L. Voegtlin, a gastroenterologist, introduced the concept of the Paleo Diet, in his book entitled, Stone Age Diet: Based on In-depth Studies on Human Ecology and the Diet of Man.
The Paleo Diet is sometimes referred to as the Paleolithic Diet, Primal Diet, or Ancestral Diet. Evidence suggest that foods that were regularly consumed by our human ancestors during the Paleolithic time period (approximately 2.6 million-10,000 years ago) may be beneficial for the prevention and treatment of some of our modern day chronic diseases. It has been suggested that the changes in our diet with the advent of farming and also the Industrial Revolution, are too abrupt for our genome to have adjusted. In developed countries today, at least 70% of the daily energy intake is from foods that were rarely or never eaten by Paleolithic hunters and gatherers. These include foods like grains, dairy products, as well as refined sugars and processed fats. Sugars and grains with a high glycemic load now represent a dominant part of the modern diet, however they were seldom consumed by humans, even as recently as 200 years ago. Observational studies of hunter-gatherer populations support the idea that a Paleo-type diet may reduce the risk of metabolic disease, type-2 diabetes, cancer, and cardiovascular disease (14).

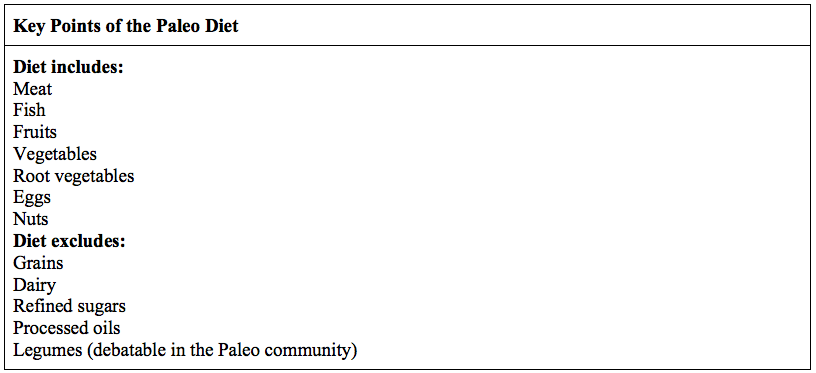
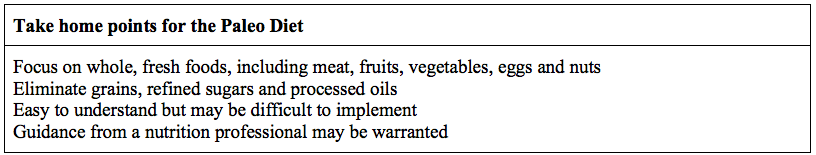
The Components of the Paleo Diet
The Paleolithic food groups include meat, fish, shellfish, fresh fruits and vegetables, roots, tubers, eggs and nuts. Highly refined grain products, processed sugars, industrial seed oils, and dairy products are not components of a Paleo diet. The diet advocates that protein be the source of 30% to 35% of daily caloric intake, and that high fiber be consumed (45-100g/day) from non-cereal based plant sources (15). There is often debate in the Paleo community regarding whether potatoes and legumes should be included in the diet.
Benefits of the Paleo Diet
Intervention studies demonstrate favorable changes in disease risk factors after the adoption of a Paleo diet, such as blood pressure, lipid profiles, glycated hemoglobin (HbA1c), glucose tolerance, insulin secretion, insulin sensitivity, weight, waist circumference and C-reactive protein level (a marker of inflammation) (16). The Paleo diet provides satiety, which can help in weight management, and it can also improve symptoms in those who suffer from gastrointestinal complaints.
How the Paleo Diet Helps Pain
Chronic Fatigue
An improvement in Chronic Fatigue symptoms has been demonstrated with the implementation of an ancestral diet. Weight loss, increased energy, less pain and fatigue, lower blood pressure and reduced anxiety are some of the positive benefits (17).
Obesity and Diabesity
Overweight patients with impaired glucose tolerance or type-2 diabetes who were put on a Paleolithic diet, decreased their leptin levels by 31%, reduced their weight as well as their waist circumference. Leptin is a peptide hormone secreted from adipose tissue, which influences appetite, blood pressure and energy homeostasis. An increase in leptin results in a decrease of food intake, however many obese people may become leptin resistant. A Paleo diet may help to normalize leptin levels (18). Diseases of insulin resistance, including metabolic syndrome, type-2 diabetes, hypertension and coronary heart disease, are commonly referred to as “diseases of civilization”, and are rare or absent among hunter-gatherer societies (19). In a randomized cross-over study, patients with type-2 diabetes were put on a Paleolithic diet during two consecutive 3-month periods. There was improvement in glycemic control, with a lowering of the HbA1c, along with a reduction in weight, blood pressure and waist circumference (20).
Observational studies of hunter-gatherer populations support the idea that a Paleo-type diet may reduce the risk of metabolic disease, type-2 diabetes, cancer, and cardiovascular disease Share on XInflammatory Bowel Disease and Irritable Bowel Syndrome
Inflammation of the gastrointestinal system can precede and predict GI issues as well as obesity. Gut inflammation is associated with increased intestinal permeability and changes in the microbiome. Bacterial overgrowth may result in increased intestinal permeability which has been associated with the pathogenesis of IBD (21). It has been shown that the microbiome of those people in countries with less Westernized diets produce microbial communities that are markedly different from those seen in industrialized countries (22). There appears to be a link between the change of food habits and food production and the incidence of IBD. Experimental studies show that some common food ingredients can alter the intestinal barrier, causing inflammation. A number of complex carbohydrates that are added to foods, such as maltodextrin, emulsifying agents, carrageenan and xanthan gum are shown to disrupt intestinal homeostasis. These products are not allowed on the Paleo diet. A stricter version of the Paleo diet, the Autoimmune Protocol, has shown to improve symptoms of IBD (see Autoimmune Protocol below) (23). There is much anecdotal evidence showing the beneficial effects of the Paleo diet on gastrointestinal conditions such as IBD, and interesting studies are continually underway (24).
Autoimmune disease
The Paleo Diet holds promise for ameliorating autoimmune diseases due to its anti-inflammatory principles. The removal of grains and processed grain products in the diet has a beneficial effect on the intestinal microbiome. If the microbiome is unbalanced, it can set the body up for developing an autoimmune condition. A Paleo diet rich in healthy protein, fat, and carbohydrates in the form of fresh whole vegetables and fruits, along with naturally fermented foods, will prevent intestinal hyperpermeability (25).
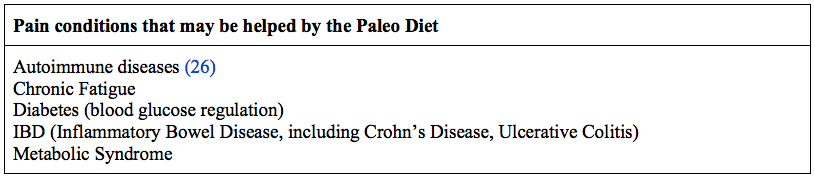
Focusing on whole, fresh and unprocessed foods, the Paleo diet reflects the way our ancestors ate. The diet is fairly easy to understand, but may be difficult for some to adhere to, especially given the amount of grains in our present food supply. Assistance from a nutrition professional is a wise idea for those with a chronic disease.
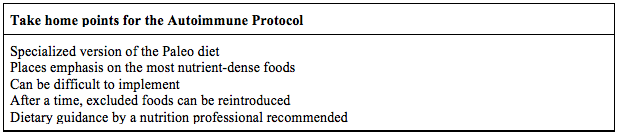
The Autoimmune Protocol
The Autoimmune Protocol (AIP), sometimes referred to as the Autoimmune Paleo Diet, is a specialized version of the Paleo Diet, whose aim is to reduce inflammation in the intestines. At its core, AIP is an elimination diet. However, some elimination diets are not complete enough and may not fully remove the triggers that cause gut inflammation. Many who suffer from autoimmune diseases have had success in relieving symptoms by adopting the AIP diet. Experts recommend staying on the diet for about a month or until improvement is seen. Then eventually some of the restricted foods can be reintroduced as symptoms subside.
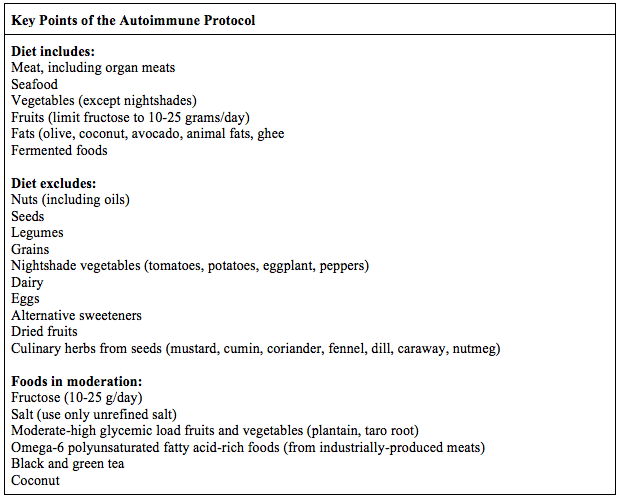
The Components of the Autoimmune Protocol
Like the Paleo diet, the Autoimmune Protocol restricts grains, dairy, and legumes, but goes further and does not allow eggs, nuts, seeds, nightshade vegetables (tomatoes, potatoes, eggplant, peppers), as well as non-nutritive sweeteners (including stevia). Foods allowed only in moderation include fructose (10-25 g/day) from fruits and starchy vegetables, salt (use only unrefined salt such as Himalayan pink or Celtic sea salt), fruits and vegetables that may have a higher glycemic load (such as dried fruit, plantain and taro root), and conventionally-raised animal meats that typically have a higher percentage of the omega-6 fatty acids (27). The caffeine in coffee and tea can affect adrenal function, so it is limited in the Autoimmune Protocol. Coconut should be used in moderation on the AIP diet due to the higher fructose fiber (inulin) it contains. In excess, it may cause intestinal bacterial overgrowth.

Foods to include on the Autoimmune Protocol consist of healthy meats, including organ meats, seafood, vegetables (except nightshades), fruits, fats and fermented foods.
Benefits of the Autoimmune Protocol
Many of those who implement the Autoimmune Protocol report a lessening of their chronic disease and autoimmune symptoms. Functional medicine practitioners and nutritionists using AIP for their patients observe improvement of chronic disease symptoms, hormone rebalancing, and the healing of increased intestinal permeability (or leaky gut) (28). Anecdotal and peer-reviewed evidence support relief from conditions such as Hashimoto’s disease, Sjogrens, and Rheumatoid Arthritis (29) (30).
Dr. Tatta’s simple and effective pain assessment tools. Quickly and easily assess pain so you can develop actionable solutions in less time.
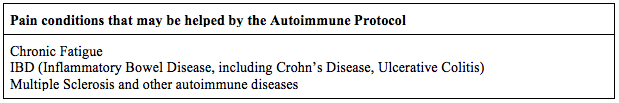
How the Autoimmune Protocol Helps Pain
Chronic and autoimmune diseases are a result of an overactive immune system, which leads to chronic inflammation. The conditions differ simply in the part of the body that is under attack by the immune system. The Autoimmune Protocol is an anti-inflammatory diet, which, when implemented, will help to reduce the inflammation that is causing an imbalance in the body, and the pain that accompanies it.
Multiple Sclerosis
A 2014 study conducted by Dr. Terry Wahls, who reversed her Multiple Sclerosis (MS) symptoms with her version of the Autoimmune Protocol called the Wahl’s Protocol, found that a multimodal intervention that included an AIP diet, significantly improved fatigue in MS patients (31). Progressive muscle weakness and chronic fatigue are chief complaints in patients with MS, leading to a decrease in physical activity and increased disability. Nutritional status has a major impact on cognitive function, brain volume, and nerve function, and is likely very important in people with MS (32). Green leafy vegetables, sulfur-rich and brightly colored vegetables and fruits present in the AIP diet, provide many of the important dietary molecules such as flavonoids, polyphenols and thiols that can impact molecular pathways reducing the disease activity and pain of MS (33).
The Autoimmune Protocol is an anti-inflammatory diet, which, when implemented, will help to reduce the inflammation that is causing an imbalance in the body, and the pain that accompanies it. Share on XChronic Fatigue
Improvement in fatigue has been observed with the implementation of an autoimmune protocol type of diet. Additional foods that may cause sensitivities are removed in the AIP diet, such as nuts, seeds, eggs and fermented foods which can trigger histamine responses leading to brain fog and fatigue in some people (34).
Inflammatory Bowel Disease and Irritable Bowel Syndrome
A study published in 2017 in the journal, Inflammatory Bowel Diseases, demonstrated that dietary modification with an AIP diet can improve the clinical responses in Inflammatory Bowel Disease. The subjects underwent a 6-week elimination followed by a 5-week maintenance phase. The Mayo score (a rating for the severity of Ulcerative Colitis) significantly improved, as did the Harvey-Bradshaw Index for Crohn’s disease. Fecal calprotectin levels improved as well, indicating a reduction in the inflammation in the intestinal mucosa. In addition, improvements were noted in the intestinal lining during follow-up endoscopies (35).
Autoimmune Disease
Like the Paleo Diet, the Autoimmune Protocol is anti-inflammatory and may reduce the symptoms of autoimmunity. It may help prevent the intestinal damage that is rampant in those consuming the modern, Western diet. AIP is a stricter version of the Paleo diet, and the few studies done to date offer hope that it can reduce the risk of acquiring an autoimmune condition.
The Autoimmune Protocol has a few peer-reviewed studies, plus a plethora of anecdotal evidence to support its effectiveness in autoimmune conditions. Additional research in this area will be most welcomed, and the protocol holds promise for those who aim to improve their chronic disease conditions with diet and lifestyle measures. This specialized version of the Paleo diet should be used as an elimination diet, with a slow reintroduction of some of the excluded foods after a given time period. It can be somewhat difficult to implement, and guidance from a health professional is suggested.
There is mounting clinical evidence that supports the idea that the food you eat can be instrumental in pain management. If you are looking for a functional or integrative way to ease your pain, you may want to try one of the diets presented in Part 1 and 2 of our series. As always, if you need a helping hand on your journey to health, don’t hesitate to contact me.