Welcome back to the Healing Pain Podcast with Dr. Navaz Habib, DC
We’re going to take a deep dive into how the vagus nerve can help reduce pain and control inflammation. Joining us is Dr. Navaz Habib. He is a functional medicine practitioner, author and speaker who empowers his clients to dig a little bit deeper and find the answers to what’s holding back their health. His office, Health Upgraded, works with entrepreneurs, executives and professional athletes who want to take their health to a new level, allowing them to contribute and serve more people. Having gone through his own personal experiences with poor health and weight struggles, Dr. Habib is well-equipped to implement personalized recommendations for each of his clients in identifying the root causes of health imbalances and addressing them naturally. His patients experience optimal health the way their bodies were meant to feel and function. On this episode, Dr. Habib is going to take us into the structure, the physiology and the function of the vagus nerve.
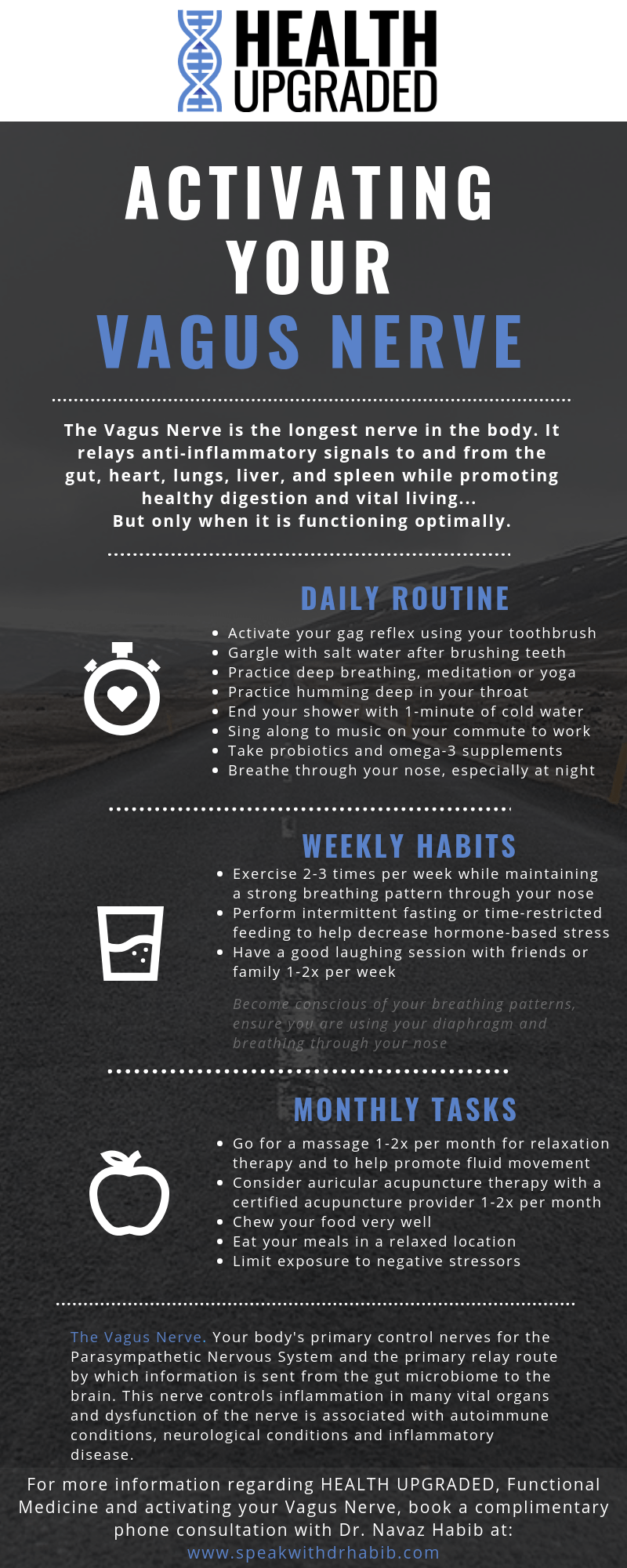
To help you out with this episode, he’s included a great little cheat sheet called Activating Your Vagus Nerve. Inside this cheat sheet, he takes you on a journey of what you can do daily, weekly and monthly to activate your vagus nerve. This is great if you’re someone who struggles with chronic pain or inflammation. It’s also a great cheat sheet to provide your patients. If you’re a practitioner, this is something you want to get your hands on. To download this cheat sheet, all you have to do is text the word 148Download to the number 44222 or you can type in the URL IntegrativePainScienceInstitute.com/148download. I’ll send that right to your inbox for free. This episode is filled with take-home strategies that you can start to use either in your practice or for your personal health. If you’re an anatomy geek like me, it’s so much fun to talk about these topics and explore or revisit what the vagus nerve does and how it’s important in helping you with that parasympathetic response. Let’s begin and let’s meet Dr. Navaz Habib.
—
Watch the episode here:
Subscribe: iTunes | Android | RSS
Using The Vagus Nerve To Reduce Pain And Inflammation with Dr. Navaz Habib, DC
Navaz, welcome to the show. It’s great to have you here.
Thank you so much for having me, Joe.
I know we’ve been planning this for a while because we first met way back in early 2019 at the Integrated Healthcare Symposium. We happened to attend the lecture together and then we went out to dinner together. You started telling me about your story and how you got into the vagus nerve, which we’ll talk about in this episode, but also functional medicine in general. Tell how you got involved in functional nutrition and functional medicine.
I’m a chiropractor by profession and so being in the healthcare space, I’ve always known that this was where I wanted to be. I wanted to be working with people, helping them feel better, get out of pain, get out of the health issues that they were dealing with. What ended up happening was I was working at a clinic in near Toronto where I live and it’s the most chance occurrence where somebody walked into my life in the most opportunistic way. It was a gentleman by the name of Sachin Patel who introduced me to functional medicine. Sachin, being as gracious as he was, showed me the ropes and showed me how I could improve my own health.
During that time, I was actually dealing with my own health challenges. I weighed 250 pounds. I was dealing with high blood pressure and high blood sugar. I had significant IBS. I had a lot of issues going on with my own health, and yet I’m this doctor that should be able to get all this information out to his patients and help them. I wasn’t able to help myself. When functional medicine and when Sachin came into my life, I was able to see what I was missing and address the missing pieces of my puzzle. I ended up losing a bunch of weight. More importantly, I got so much healthier. I feel so much better. That’s what brought me into it because once I was able to use this system to fix myself, it was a no brainer. It was time to get this out to as many people as I possibly could.
You mentioned you lost a bunch of weight, but as reading through some of your information, doing some research on you, you lost over 75 pounds.
I lost about 75 total pounds.
It is a tremendous accomplishment. Few people are able to lose that much weight and keep it off. This is not true for everyone, but I do think it’s important to some extent that practitioners have to walk their own walk. It’s like, “How can I do this if you’re not doing this??” That doesn’t mean that as practitioners we don’t have our own health challenges. We definitely do. I’ve had mine and I’ll probably have another one in my lifetime and you probably will too. It’s part of being human on our human course of health. Let’s segue into that and tell me how you got involved. Functional medicine is a huge field. There are so many different areas in places you can go down into, but you wrote a book called Activate Your Vagus Nerve. You became very interested in the vagus nerve and its influence on health. We’ll talk about pain and inflammation, but how did the vagus nerve come to the surface and say, “You may want to go into this deeper?”
I’ll say that it all started when I was in chiropractic college. I was always very interested in nerves and understanding how the nervous system works and understanding the flow of energy and information from the brain to the body. There was always a bit of an underlying understanding that there are a lot of things in the body that we are yet to fully understand and fully comprehend. Yet there were things like the vagus nerve where we’re told it’s parasympathetic. I’ll talk about what that means. In school, we’re told it’s one thing and yet when you go into the research, it shows that there’s so much more to this. I became interested in it more when I was working with many of my patients. I noticed that there was a lot of similarities, a lot of commonalities between different types of conditions, but all of them being inflammatory in nature, having some inflammatory process in nature.
I always was wondering, if there’s so much inflammation going on, what is there available to control it? How does our body normally control this inflammation? What is there to stop that? That’s what brought me into the vagus nerve and into the realm of more than what vagus nerve does to control inflammation. What does it do in managing digestion and managing our detoxification processes? What does it do in managing our pancreatic function, managing our kidney detoxification and sending information from the microbiome to the brain? It revolved into this thing where I said, “I have to get this information out,” then the book came to be.
For those who have not taken neuroanatomy, give us a little vagus 101 neuroanatomy lesson on where it originates, where it innovates and vice versa.
The central nervous system is made up of the brain and the spinal cord. When we generally think of the brain in lay people’s terms, it’s the brain and the spinal cord. That’s the central nervous system. Where do those nerves come from? That’s where the important thing comes up here. We have twelve pairs of cranial nerves, one nerve on each side becoming a pair. Cranial nerves are numbered from cranial nerve one through twelve and all of the cranial nerves except for one will stay within the cranium, which is the head cavity area. That one, cranial nerve number ten called the vagus nerve is the one that actually will leave the cranial cavity and go to other places. It doesn’t just go to other places. That goes to more places than any other nerve in the body.
It’s one of the longest nerves in the body. It has one of the most diverse amounts of information that’s going to be transported on it. It originates in the neck, just behind the ears a little bit. It comes down, sends a branch to the ears, which we’ll talk about. It sends a branch to the muscles of the back of the throat and to the voicebox. In fact, the reason I can speak and have pitch and tone in my voice is because of the vagus nerve. It sends signals to the heart, to the lungs and down into essentially every organ of our abdomen as well. It’s the entire digestive and detoxification tracks and all of those as well. It’s called the vagus nerve. The word vagus comes from the root word vague, which is wandering, meaning it goes to so many different places. I talk a lot about what anatomists were thinking when they were initially looking at this and saying, “My goodness, this goes so far. We need to call it something and we don’t know what to call it. It’s so vague. Let’s call it the vagus nerve.”
I love the little play on words there. You study anatomy. It’s important to look at the Latin roots of things. They do actually tell you a lot about how the structure and function of the different parts of your bodywork. Tell us about inflammation first. Tell us about how the vagus nerve helps us modulate inflammation.
Inflammation in our body comes up due to various reasons. It can be due to gut imbalances, it can be due to acute trauma, it can be due to a concussion, whatever. There are so many different ways that inflammation levels are raised. What the vagus nerve does is it has this very specific acetylcholine as the neurotransmitter that it uses. Acetylcholine is the major guy. ACH is what we call it in clinical terms. The cholinergic anti-inflammatory system is modulated through the vagus nerve to help control inflammatory levels, to help control inflammation. If we’re not able to send out the acetylcholine and get that system working well, that inflammation levels can’t be modulated or be managed and so they start to rise. That’s where we tend to get these major issues where inflammation levels are way too high, leading to chronic pain and issues that are going on with so many conditions that we know of.
The vagus nerve secretes acetylcholine, which tends to have an anti-inflammatory effect in the body. What would prevent the vagus nerve from secreting that acetylcholine? Obviously it does this naturally, but there must be things in our environment that prevent us from doing that.
Like every other nerve in our entire body, nerves need to be exercised. They need to be used, they need to work correctly. People that are dealing with muscular issues tend to not actually have issues with muscles. They have issues with the nerve that’s sending information to that muscle. If we don’t train that nerve, then that muscle can’t build up. We’ll put it in very simple terms. For example, somebody who does bicep curls very often is going to grow a very big bicep, but it’s not the fact that they’ve grown the big bicep. They’ve sent that signal down that nerve and exercised that nerve significantly enough to allow that muscle to have a strong level of function. That strong level of function can be brute force or it can also be very minute fine-tune little things as well, but just like that, every nerve in the body, including the vagus nerve needs to be exercised.
It needs to be trained and worked and needs to be used. When we stop using it correctly, we tend to have these issues. There are so many different reasons why the vagus nerve could not work correctly. It can be simply the fact that we’re chewing too quickly, not eating our food correctly and sending no signal down to the rest of the digestive tract that, “Food is coming. You need to be ready for it.” It could be and this is an interesting one that came up from one of my teammates, from one of my team members who in the past was dealing with a very significant eating disorder. Bulimia was leading her to bring her food back up. What that meant was the digestive tract and the digestive system was not working in the uni-directional pathway that it was supposed to.
She was stimulating the gag reflex but causing food to come back up the other way. That would very negatively affect the vagus nerve. It can also be cut during surgery, which is common. Sadly now there’s some research out there and some newly approved methods that they’re actually cutting the vagus nerve. They’re doing a vagotomy to prevent or to slow down Alzheimer’s disease, which is ridiculous because where’s it coming from? It’s funny to see that we’re still heading down that path. There are many ways that vagus nerve can be injured or have its effect and its positive power slowed so that it’s not able to do the job that it needs to do.
Take me back to that point of a vagotomy. What’s the rationale behind that?
The idea is that Alpha-synuclein is being actually produced. Alpha-synuclein, you can almost think of it like a prion. Its almost like Mad Cow Disease type of thing and the plaque that’s formed in there is the same type of plaque that is now being found in the brains of people dealing with Parkinson’s. We’re finding now that Alpha-synuclein that plaque that’s forming in the brain is moving up through the vagus nerve to the brain. The question isn’t, “Let’s cut the vagus nerve and stop the Alpha-synuclein from coming up.” The question should be, “Why is that Alpha-synuclein getting into the vagus nerve? Where is it coming from?” The answer to that, as we know in functional medicine, is from the gut 100%. It’s from dysbiotic gut bacteria, from issues that are going on with core digestive tracts, from poor food choices. That’s leading to this extra inflammation that’s leading to this Alpha-synuclein buildup that’s leading to this Parkinson’s. It’s not the fact that we need to stop vagus nerve from functioning too.
It’s interesting that we landed on that. It’s the difference between a biomedical model versus a functional medicine model because let’s say you did cut the vagus nerve, which I don’t recommend anyone do that. There are other ways for substances, let’s just say, to get into your nervous system, i.e., your brain through the blood-brain barrier, through your circuitry system, through your lymphatic system, through other nerves and pathways. It’s interesting that they would go that route and not to say it doesn’t help some people. It probably does, but it’s not getting to the root cause of exactly what’s there. As far as the vagus nerve not functioning optimally, what are some of the ways that people show up to look towards helping their vagus nerve function optimally?
There are a lot of different things. In order for us to truly understand the best ways to improve vagus nerve function, we have to look at what are the functions of the vagus nerve to begin with? I talked about where the nerve goes and that’s what we can get into here. There are four different functions of the vagus nerve that we need to know of. The first one is the one that everybody believes that is the major most important one, and that is the parasympathetic function. What is parasympathetic? What does that even mean? Our body has certain automatic processes that are ongoing. I’m not consciously thinking about beating my heart at this moment. I’m not consciously thinking about every breath that I’m taking. I’m not consciously thinking about detoxifying the food that I’ve eaten or whatever. Those processes are happening automatically.
This is using what’s called the autonomic nervous system. The autonomic nervous system has two branches. It has a sympathetic and parasympathetic. The sympathetic side is the survival mechanism, the fight and flight side. It’s a necessary component. It needs to be there in order for us to survive, especially when it comes to car accidents. When it comes to significant traumatic events, when we are able to function during those situations, our stress levels rise. Our survival mechanisms kick in, but we can’t be in that survival mechanism road all the time. What that survival mechanism is going to do is it’s going to raise our heart rate significantly. It’s going to shallow our breath. That’s going to make our breath very shallow and not very calm and relaxed. It’s going to shut off the digestive system because if you’re trying to run away from a traumatic event like being chased by a dog or a sabertooth tiger way back in evolutionary times, we have these survival mechanisms that need to be produced because digestion doesn’t work.
We need to send that blood flow to the muscles. Muscles in the arms and legs get the extra blood flow and the function is moving. That’s necessary for certain stages, but the vast majority of the time we shouldn’t be sitting in a relaxed rest digest state. That’s the parasympathetic side, the side that’s modulated majority of the body through the vagus nerve. That function is very important. However, here’s the fun tidbit. We all think that the vagus is parasympathetic. It’s only 15% of the information that’s transmitted over the vagus nerve is parasympathetic activity. It’s very interesting to know that that’s what we think and yet 80% of the information is the second function. That’s afferent. That’s function being sent information from the gut, from the lungs, from the heart, from the liver, from all of the organs that it integrates to the brain.
It’s a status update. It’s telling our brain what’s going on. It’s letting our body know what’s going on or letting our brain know what’s happening in every organ of our body in order to maintain that level of homeostasis. If we’re not able to do that, send that information up, then we have a big issue. That’s 80% of the information there. I know we have a lot of information. You’ve put a lot of stuff up on the emails on microbiome information and the relay of information from the gut to the brain. This is the major physical highway for that information to get up through the vagus nerve.
I love it because we talk so much about safety on this show, helping the human body feel safe. When a human body feels safe, oftentimes chronic pain can be alleviated that way. What you’re saying is the vagus surveys all the different major organs in our body, brings that information up to the brain and the brainstem and gives that information. Your brain can then make a decision on it. If we give it some context, when you have anxiety or public speaking is probably the easiest one to talk about. When you feel that tightening in your chest, when you feel short of breath, when your stomach starts to ache and you get butterflies in your stomach, your heart starts to rise, your blood pressure increases, that’s all the vagus nerve at work.
In fact, in that situation, it’s shutting down. The information is being decreased, but it’s telling your body, it’s telling your brain what’s going on. It’s relaying the information of what’s happening inside of those. The parasympathetic activity is shutting down, but the afferent information is coming up. It’s telling you exactly what’s going on. That’s a great way to look at it.
It puts you in that fight or flight. Give us some tips of strategies of how we could modulate the vagus nerve on our own. We can talk about exercise first since it’s an important point factor in health overall. What type of exercise would help stimulate the vagus nerve beneficially?
This is a great important piece of information. The majority of my patients are high-performing executives, entrepreneurs, people that are dealing with stressful lives outside, but they’re able to come back then and get back into a recovery state. That’s what I help people do is get back into that recovery state. People that aren’t doing constant physical activity like a professional athlete, for example, are going to need to do exercises that are not overly intensive. It’s a constant daily movement that makes more of a difference than exercise for 30 minutes a day and then just sitting on your butt for the next eight hours.
Optimizing vagus nerve function can help alleviate pain and inflammation. Share on XWe need to do something where there’s movement occurring all the time. Think of it this way. If our joints were not moving, we would not be able to lubricate them. We would not be able to get nutrients to our joints. If we have for example, joint pain, as a chiropractor, I’ve seen tons of this and as a physio, I know you’ve seen a ton of it as well, joints don’t have a blood supply to them. Joints get their nourishment from the synovial fluid, from the fluid being moved around. If the joints are not moving, then that synovial fluid isn’t getting pumped in and out and we’re not able to get those nutrients that are necessary to those joints. I have people do things that they find are not going to stress them out, exercises that help them get into a calmer state.
A lot of people enjoy running or biking because it almost takes them into a meditative state. That’s something that I enjoy. I go for my morning bike ride a couple of mornings a week, at least in the summertime. I’m able to get outside, get into a bit of a calm breathing state, but I’m still pumping my legs and feeling like I’m getting things moving. That’s something that I get people to do a lot of. Find an exercise. Find a movement pattern that calms you down while still physically causing you to move. Something like running, something like even gently going for walks and getting those joints moving. If the pain is too severe, walks are probably one of the best things that you can do for yourself to help with that. If you’re sitting at a desk, oftentimes now that we have computer jobs and whatnot, if it’s possible a standing desk. If it’s not possible, get something where you can raise your computer up to a height on top of the desk where you can then stand and sit for 10 minutes, 15 minutes, 30 minutes a day or 30 minutes each hour, even if it’s possible. Allow yourself to be in different positions while still being in a calm state.
Are there mindful movement practices that there’s literature supporting the regulation, the modulation of the vagus nerve for health?
100%. A lot of what I talk about in the book and a lot of the research that I came across actually talked a lot about traditional Chinese medicine, Ayurvedic medicine and the tools that they’ve been using for millennia for thousands of years to get our bodies working at absolute optimal. Yoga was one of the top things that people could do. Tai chi is a wonderful mindful movement practice. Qigong is another wonderful mindful movement practice. These have been going on for thousands of years. We’re in the last ten to fifteen years understanding that these things are not just about exercise and movement.
They have significant restorative effects on our own health as well. If you think about yoga and pilates, the focus of these movements is actually back to the breath, allowing the breath to be the focus and then putting yourself in different difficult positions while you’re still focusing your attention on the breath. I’m a huge proponent of yoga, pilates, tai chi, qigong, any of those mindful movement type things where you’re not overly straining the body but allowing yourself to move while being in a calm state. Those are huge and very popular. I do talk about them a bit in the book as well.
Moving into digestion, how important is it to look at nutrition, diet, eating with regard to vagus nerve function?
There is so much information and so much importance that needs to be put towards this. I talked in the book about the fact that there isn’t a single diet for anybody for the entire planet. Not everybody needs to be ketogenic. Not everybody needs to be vegan. Certainly, there are people that will thrive in each one of these things and it is completely up to each person as to what they want to do, whether it’s unethical or whatever decision that they’re making. I have this simple idea based on the type of agriculture and type of food industry that we tend to live in. I choose three things, green, clean, lean. Green being choosing the vast majority of your food being greens that come from the ground, things that are natural, organic, and that’s where the clean comes in.
Organic is key because who knows what we’re spraying on things nowadays. Even the organic stuff tends to have a little bit of this stuff, the glyphosates and the toxins that are building up these pro-inflammatory toxins. It’s green, clean and lean. I talk about lean in terms of the meats that we tend to be choosing. A lot of the inorganic, the regular conventional based foods, the meats, the beef, pork, chicken, tend to have a lot of fat on them. It’s because those fats should not have been there in the first place. We’re not built to have a ratio of high Omega-6 and low Omega-3’s. We need to have a good ratio.
These foods, these chicken and conventionally raised beef and whatnot have very high levels of Omega-6 because of the food that they’re eating. Think about it this way. The food that you’re eating, the meat that you’re eating has eaten something. If they haven’t eaten well, you’re not eating well and so that’s why I say go with the lean meat where possible and then add in good fats. Add in the good avocado, coconut oil, olive oil, get in those good omega-3 fatty acids. Get those guys in because they’re going to make a big difference to you. The fish oils will make a huge difference. I know that’s something that will be a huge, very positive effect in inflammation modulation and improving the Omega-6 to Omega-3 ratio significantly.
Does the vagus have a direct influence on certain types of hormone modulation?
Not a direct effect. It is indirect. It does not seem specific to cortisol or whatnot, but it does have certain ones in terms of the pancreas. Insulin specifically is going to be modulated somewhat through vagus as well. The vagus nerve sends a lot of signals to and from the pancreas. The pancreas is going to react and return to what’s happening with blood sugars. The blood sugars are actually being sensed in the liver. The liver is going to sense the blood sugar and send a signal to the brain saying, “The blood sugars are getting high, send more insulin,” and it’s going to send information down to the pancreas saying, “Please send this out.” In terms of sex and stress hormones, it’s not involved. It’s more involved in the digestive and metabolic and blood sugar based hormones.
It’s still amazing how many different types of innovations and actions and how it influences your overall health and well-being. We talked a little bit about exercise and nutrition. We touched on hormones, you spoke about diet a little bit. How can we access it? The vagus stories are internal. It’s coming from your brainstem. I can’t put my hands on anyone’s brainstem necessarily. Is there a way for us to access the vagus nerve on the peripheral part of our body?
There are some things that we can do and there are actually a lot of devices that are coming out that are very interesting in being able to stimulate the vagus nerve exogenously not from what we can do. I’ll talk a little bit about what we can do afterward as well. Interestingly in terms of the anatomy, the vagus nerve in the neck is where we have true access to it and this is an important piece of the health puzzle and the vagus nerve puzzle. In the neck on each side, we have a carotid artery and the jugular vein that go through a sheath or a little package in the neck. That’s a protective coating for those two blood vessels. Those are the blood vessels that take blood to and from the brain, the main ones. In that carotid sheath is one more item and that is the vagus nerve.
It should go to show you how important the vagus nerve is when it’s sitting with the carotid and the jugular. It’s that important, but that’s exactly where we can have that physical function or physical attachment to it. It goes right from behind the ear a little bit there. It’s what’s called the mastoid process. It’s right behind that, just down along the sternocleidomastoid muscle, STM. Right in front of that, right where we feel the pulse essentially is where we can actually affect the vagus nerve from the outside. You’re looking for that specifically as you’re palpating around the neck area. That would be the key. If you can find the heartbeat, if you can find the pulse going on in the carotid, then you’re very close to the vagus.
There’s manual therapy on the cervical spine to help influence and modulate the vagus nerve on some level. When I think about this, you can obviously have soft tissue techniques to do on the cervical spine. There are mobilization techniques, there are manipulation techniques, lots of different techniques that all different types of manual therapists use. Are they influencing the vagus nerve indirectly or sometimes if they know what they’re doing, potentially directly?
There’s a lot of great information on this and so the best way for us to know that we’re having an effect on the vagus nerve is to measure the function of the vagus nerve. That is done through looking at what’s called heart rate variability. We’re not looking at heart rate. We’re not looking at how fast or how slow your heart is beating, although that does have a bit of an effect from the vagus nerve. The heart rate variability, that time of variation between intermediate or between beats, it’s what’s called the interbeat interval. It’s the time between each beat of your heart. If there’s variation, if there’s a high level of variation from one beat to another over a period of time, then that is a very good sign that the vagus nerve is functioning well.
 It should not be rhythmic and not have a lot of variation. If that’s happening, that means that the vagus nerve is not being able to send a lot of information and that sympathetic innovation to the heart is working much harder and much better. Where if we have that intermediate interval that’s shifting a little bit, anywhere between 50, 60, 70, 100, 120 milliseconds of variation between the intermediate intervals, then that’s a very good sign that the vagus nerve is working well. In order to improve that, there are manual techniques that work well. There have been measurements done and studies were done showing that heart rate variability does increase with manual therapy of the cervical region for sure.
It should not be rhythmic and not have a lot of variation. If that’s happening, that means that the vagus nerve is not being able to send a lot of information and that sympathetic innovation to the heart is working much harder and much better. Where if we have that intermediate interval that’s shifting a little bit, anywhere between 50, 60, 70, 100, 120 milliseconds of variation between the intermediate intervals, then that’s a very good sign that the vagus nerve is working well. In order to improve that, there are manual techniques that work well. There have been measurements done and studies were done showing that heart rate variability does increase with manual therapy of the cervical region for sure.
Soft tissue therapy does have some effect. It’s not as strong as manipulative effects of like C0/C1, C1/C2 of the upper cervical spine. Those tend to have very high effects on heart rate variability, although you need to pick and choose who you’re doing that with from a practitioner side. There is some information that needs to be done on an individual basis when you get there. The other interesting study that I’m thinking of is there was a great study that showed mobilization of the upper cervicals between C0/C1 and C1/C2. It had a very strong effect on decreasing blood pressure as well. That blood pressure is something that’s monitored through vagus and so if we’re able to reduce that, then that means that we’re able to modulate the function of vagus using manual techniques of the upper cervical spine.
It’s interesting because the vagus nerve doesn’t intervein C0/C1, C1/C2, does it?
It does not. I believe it has to do with the muscular intervein from C0/C1 of the suboccipital and that affecting everything in the carotid, in the neck, cervical spine, how tense are the muscles of the neck affecting vagus nerve that way. It’s an indirect effect on vagus through them.
It’s a fascinating connection though. Talk to me a little bit about vagus nerve stimulation using electrical stimulation. I know there are some people, if you go out into the internet, into the waves and look, there are some people looking into this and saying it might this be beneficial for stress or even things like weight loss I’ve read things online. Talk to us about what you know about the research there and if someone under the guidance of a practitioner wanting to do this, what does it entail?
There are a lot of tools that are coming out nowadays where we’re trying to do this and there are certain ones that are FDA-approved and able to be used for certain things. The name of the one that I’m thinking of is slipping my brain, but it’s one that you can literally attach to your neck, hold it there for a couple of minutes. It does electrical stimulation to the vagus nerve and it has been shown to have very positive effects on headaches, migraine specifically. It’s definitely cleared for that one. It’s an interesting tool and the biggest nerve stimulation using electrical stimulation is great when it’s necessary. I personally am a big proponent of stimulating the vagus nerve using endogenous techniques, using ways that we know that the vagus nerve can function.
I spoke about the four functions of the vagus, I missed out two of them. The sensory aspects of the skin of the inside of the ear are actually innervated by the vagus nerve. One of the best tools that I have people do is where they need a positive effect is to go and get acupuncture or acupressure done for that area. That has such amazing positive effects. I know I practice acupuncture a little bit as well. I’ve studied it and the effect of putting a needle into that exact spot and having everybody calm right down is profound. It’s amazing. Only about 1% to 2% of the information on vagus is that sensory aspect. However, if we’re getting any stimulation of the vagus nerve through that way, through that pathway, then we’re able to affect the positive information pathways of the parasympathetic and the afferent function as well. Make sure that is working. It’s essentially an exercise for that.
The last one, the fourth one is the muscles of the larynx and the back of the throat, the pharynx. Keeping the airway open, not snoring at night, is something that changed a lot when I lost my weight because I stopped snoring. I was able to breathe through the night and now through my nose overnight, which is actually optimal for not only my oral health but really good for my vagus and its function and getting my heart rate variability up. It’s something I measure using my Aura ring at night, which is amazing. What we can do now is keep those muscles and the back of the throat open so that the airway can be patent and allow air to go. I said a little bit about the vocal cords and the fact that the muscles of the larynx are innervated by vagus as well.
This is where we can really have positive effects on a daily basis for each person for free, simple tools that we can use to stimulate vagus nerve function. Gargling, gag reflex, humming, chanting, things that we do to stimulate a vibration in the vagus, innervated laryngeal muscles will make a huge difference. A couple of recommendations that I give to my patients is to keep a glass right beside your sink where you’re brushing and every time you brush your teeth, go ahead and gargle. Put some warm water in, throw a little salt in it, it has a great antibacterial effect, and then go and gargle.
Gargle hard. Gargle to the point where you feel the vibration occurring and then you start to tear from your eyes. You know you’re doing a good job of stimulating the brainstem and the nuclei of the vagus nerve when you start to have that tearing occurring from your eyes. Gargling hard is a great way to improve that. There have been studies that show the HRV level, Heart Rate Variability level does increase post doing that. If you do that regularly, if you do that for four to six weeks in a row, heart rate variability will maintain at that higher level. We do need to exercise that nerve and exercise that muscle to do that.
You mentioned humming. Does singing have the same effect?
Yes, absolutely. If you’re commuting to work, for example, I get people to shut the windows and belt out your favorite song and go for it. Singing will have a very similar effect to that. Listening to music overall has a great effect on heart rate variability. Funny enough, there was one specific song that actually had a greater effect on heart rate variability than any other ones that they studied. It was Mozart K 448, Two Pianos. It’s about a twenty-minute piece of music where you’re listening to Mozart. We’ve heard of the Mozart effect where we get little kids smarter. Kids are getting smarter when they listened to Mozart. He also has this effect where heart rate variability goes up and we can become calmer when listening to these specific things. It was interesting going through my research and seeing there’s one specific piece that Mozart had done that had a greater effect on heart rate variability than any other piece that he had done.
The humming, does it have to be in a certain octave, like a higher pitch or a lower pitch hum?
I don’t think there’s anything specific there, but if we think back to where that humming idea came from and who has been using it in the past, you hum at that level where it has a deeper resonance. With that deeper resonance, what you’re noticing is there’s a greater level of vibration that’s occurring and that will stimulate the vagus nerve. I truly believe that’s where “om” came from, was to help stimulate the calming effect of the parasympathetic through a physical modulation of the muscles here. Hindus, when they meditate or when they use this om, they’re actually getting into a very calm state by simply triggering that, which is one of my favorite things to tell my patients to do.
I’m imagining the audience humming and singing, “Om,” which is good. I’m glad we’re helping people. Navaz, it has been great talking to you about activating your vagus nerve. Of course, you have a whole book on it called Activate Your Vagus Nerve. You can find it on Amazon or you could go to Dr. Habib’s website, which is www.DrHabib.ca because he is in Toronto, Canada. You can find out all the information about Dr. Habib as well as of course in the book. Tell us what’s next for you. What are you working on? I know you’re building a practice in Toronto. You’re busy. What’s next?
I’m building up a practice where I’m working with professionals, professional athletes, executives, entrepreneurs, essentially anybody who wants to take their function to the next level and not have helped block them from doing that. I’m using functional medicine to do that at my clinic called Health Upgraded.
Make sure you check out his website. Make sure you purchase his book. We have a great download. It’s a little bit of information, but you can take home and you can use right away. Make sure you check out the book. I want to thank Navaz for being on the show. Thank you so much.
Important Links:
- Dr. Navaz Habib
- Health Upgraded
- Sachin Patel
- Activate Your Vagus Nerve
- https://integrativepainscienceinstitute.com/148download
- www.VagusNerveBook.com
About Dr. Navaz Habib, DC
 Dr. Navaz Habib, is a functional medicine practitioner, author, speaker who empowers his clients to dig a little deeper and find the answers to what is holding back their health. His office “Health Upgraded” works with entrepreneurs, executives and professional athletes who want to take their health to a new level, allowing them to contribute and serve more people.
Dr. Navaz Habib, is a functional medicine practitioner, author, speaker who empowers his clients to dig a little deeper and find the answers to what is holding back their health. His office “Health Upgraded” works with entrepreneurs, executives and professional athletes who want to take their health to a new level, allowing them to contribute and serve more people.
Having gone through his own personal experiences with poor health and weight struggles, Dr. Habib is well equipped to implement personalized recommendations for each of his clients. In identifying the root causes of health imbalances, and addressing them naturally, his patients experience optimal health the way their bodies were meant to feel, rather than continuing to deal with the stressors that are holding them back.
Dr. Habib’s book “Activate Your Vagus Nerve” is a simple to follow guide to help you identify and address a major missing piece in patients dealing with chronic health concerns such as anxiety and depression. By activating the Vagus nerve, we can optimize our productivity, focus and energy levels, allowing us to experience the effects of upgraded health.
The Healing Pain Podcast brings together top minds from the world of pain science and related fields to discuss the latest findings and share effective solutions for persistent pain.
If you would like to appear as an expert speaker in an episode of The Healing Pain Podcast contact [email protected].
Love the show? Subscribe, rate, review, and share!
Join the Healing Pain Podcast Community today: