About 40% of American adults struggle with some type of chronic pain syndrome, but all too often treatment is delayed, disorganized, inaccessible, or ineffective (1).
Why is this?
Pain science and pain education are under-prioritized and poorly covered topics in the education of various health care disciplines.
The 2011 Institute of Medicine (IOM) report “Relieving Pain in America”, highlighted educational deficits in the assessment and management of pain.

In order to address deficits in pain education across health disciplines, the IOM report recommends that primary education programs adapt their curriculum to focus on pain management using a biopsychosocial and interdisciplinary approach. It also defined core competencies in pain assessment and management for pre-licensure health professional education (2). These competencies are closely aligned with the International Association for the Study of Pain (IASP) guidelines for pain education curricula and revolve around four subjects :
- Multidimensional nature of pain
- Pain assessment and measurement
- Management of pain
- Clinical conditions
Because pain is one of the most common reasons that patients seek physical therapy services, practitioners need to be able to understand pain at a deep level to evaluate, treat and support their clients or patients. Physical therapists also require up to date information in preparation for leadership positions in pain care. But is the education physical therapists receive sufficient with regards to pain science education?
We continue the Pain Education blog series that started with AN INSIDE LOOK AT WHAT DOCTORS LEARN ABOUT PAIN IN MEDICAL SCHOOL and A GUIDE ON PAIN EDUCATION FOR PHYSICAL THERAPISTS, by focusing on how pain education is incorporated into Physical Therapy curricula today.
Is the education physical therapists receive adequate and sufficient with regard to pain education? Share on XHow is Pain Education Taught in US Physical Therapy Schools?
A 2015 article in The Journal of Pain summarizes results of a faculty survey that assessed the extent of pain education in accredited PT schools in the United States (3). The survey, designed by Marie K. Hoeger Bement, MPT, Ph.D., and Kathleen A. Sluka, PT, Ph.D., consisted of 10 questions addressing the following subject areas:
- Pain assessment
- Pain management
- Adequacy of pain curriculum
- Basic science mechanisms and concepts about pain
The survey also evaluated how pain was incorporated into the curriculum, the amount of teaching time given and the resources applied.
Was There an Education Course Dedicated to Pain?
The first question, answered by 76% (167/216) of schools, addressed whether pain mechanisms/management was taught through a free-standing course, or through designated time blocks within other teaching topics. Fewer schools (71%) detailed the number of contact hours devoted to these areas, and several expressed that the question was difficult to answer because pain was integrated throughout the curriculum.

Only 62% (137/216) of respondents answered questions 2 to 10, which assessed what was taught and the number of hours spent on each subject. Again, integration of pain education throughout the curriculum was cited as the reason that this portion of the survey remained unanswered.
Main findings:
- Total pain content was 31 ± 1.8 (mean ± standard error of the mean) contact hours.
- Most schools reported about 10 hours (modal value), though there was considerable variation between institutions (from 5 to 115 hours).
- Just 6% (11/167) of respondents had an independent pain course, averaging 2.3 ± 1.3 hours/semester (mode 2; range 1–5).
- Most schools (140/167) have designated blocks of time to address pain, integrated throughout the curriculum.
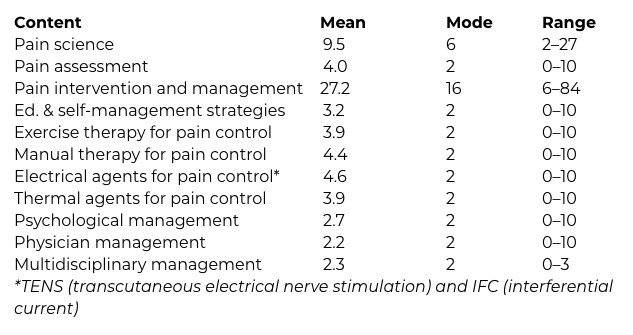
- Most teaching time was devoted to pain intervention and management (27.2 hours), while pain assessment received the least contact hours (4.0 hours)
- Within the pain science category, the majority of schools (> 83%) covered all areas. Pain pathways, acute versus chronic pain and the biopsychosocial model were the most covered science topics (>94%).
- Within the pain assessment category, subjective pain intensity rating scales (eg. numerical rating scale, visual analog scale) were taught by 99% of schools and had the highest coverage rate among all pain education areas. In contrast, pain assessment across lifespan was the least covered topic (68%).
Contact Hours in Pain Science, Assessment, Intervention & Management
Percentage of Schools That Cover Specific Pain Science and Assessment
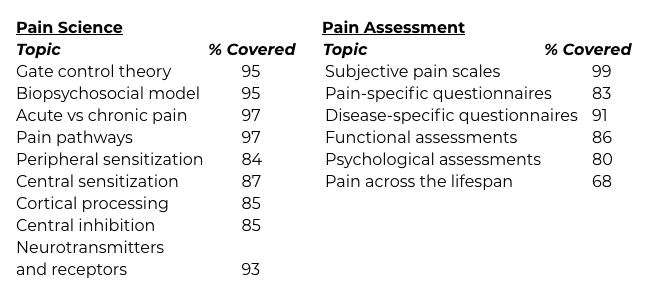
Detailed results from the survey are shown in the Tables below adapted from REF (3).
Among the resources used for teaching pain content, the following books were used most commonly, though not exclusively:
- Pain Mechanisms and Management for the Physical Therapist (18%) (4)
- Textbook of Pain 20 (17%) (5)
- Explain Pain (7%) (6)
- Bonica’s Management of Pain (4%) (7)
Reasons for Concern and Room for Improvement
Although advances were noted with respect to previous assessments for increased coverage of pain topics and use of teaching hours, the evidence indicates that pain education is still fragmented and insufficient in most Physical Therapy schools surveyed.
The survey revealed that only 61% of schools considered that ‘adequate’ pain management education had been delivered to their students. Also, less than 50% of respondents were aware of the IOM report on pain in 2011 (48%) or of the IASP guidelines for PT pain education (46%).
Dr. Tatta’s simple and effective pain assessment tools. Quickly and easily assess pain so you can develop actionable solutions in less time.
Action Steps to Improve Pain Education in PT Programs
- Awareness of, and adherence to, recommendations and educational advancements outlined in the IOM report, IASP guidelines, and the National Pain Strategy
- Implementation of stand-alone, pain-specific courses.
- The inclusion of standardized pain curriculum requirements through accreditation groups, and testing of pain knowledge and clinical competency with licensure examination
- Integration of interprofessional pain management competencies through learning activities and outcome assessment (8)
- Integration of psychosocial and cognitive-behavioral interventions.
- Integration of nutrition, CAM and lifestyle interventions.
The above changes to Physical Therapy school curricula will ensure that students enter practice with the knowledge and skills necessary to meet the full potential of the PT profession, in turn, reducing the large human and economic costs of unrelieved pain and suffering.
Because pain is one of the most common reasons for seeking Physical Therapy services, physical therapists need to be able to understand pain at a deep level to evaluate, treat and support their clients or patients. Share on XDo you have first-hand experience in pain education?
Did you receive pain education or pain science education training in school?
Leave me a comment on the Institute Facebook page!
REFERENCES:
1- IOM Committee on Advancing Pain Research Care. Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Institute of Medicine. Washington (DC): National Academies Press; 2011.
2- Fishman, S. M., Young, H. M., Lucas Arwood, E., Chou, R., Herr, K., Murinson, B. B., … & Bakerjian, D. (2013). Core competencies for pain management: results of an interprofessional consensus summit. Pain Medicine, 14(7), 971-981.
3- Bement, M. K. H., & Sluka, K. A. (2015). The current state of physical therapy pain curricula in the United States: a faculty survey. The Journal of Pain, 16(2), 144-152.
4- Sluka, K. A. (2016). Mechanisms and management of pain for the physical therapist. Lippincott Williams & Wilkins.
5- McMahon, S., Kolzenburg, M., Tracey, I., & Turk, D. Wall and Melzack’s Textbook of Pain. Philadelphia, Elsevier, 2013
6- Butler, D.S., & Moseley, L.S. Explain Pain. Adelaide, Noigroup Publications, 2003
7- Fishman, S. M. (2012). Bonica’s management of pain. Lippincott Williams & Wilkins.
8- Hoeger Bement, M. K., St. Marie, B. J., Nordstrom, T. M., Christensen, N., Mongoven, J. M., Koebner, I. J., … & Sluka, K. A. (2014). An interprofessional consensus of core competencies for prelicensure education in pain management: curriculum application for physical therapy. Physical therapy, 94(4), 451-465.



