There are two patients with sprained knee ligaments in your schedule today. One is a middle-aged man with diabetes that works as a mailman. The other, a young girl who fell while playing basketball at school. Since they share the same injury, your exercise indications will probably be similar. But would your recommendations about pain management also be the same? This article is a helpful guide on pain education for physical therapists.
Sleeping Giants: Physical Therapists as Key Players in the Management of Pain
Due to the vast number of conditions that physical therapists treat on a daily basis (where pain is a common motive) time spent with a patient and the increased frequency of patient visits per episode of care, physical therapists are uniquely positioned to not only effectively treat pain, but to prevent it, by thoroughly assessing the needs, expectations, and resources of their patients or clients (1). Moreover, as direct access to Physical Therapy services increases, physical therapists are becoming a more frequent entry point for patients into the health care system, which demands yet a bigger role in comprehensive patient care (2).
Which begs the question: Are physical therapists optimally prepared to assess, manage, and treat pain? To answer this question, let’s address a more fundamental one:

Pain Education for Physical Therapists: Is this Properly Taught?
A 2014 review contemplating this question provides a sobering statement:
“Most physical therapist education programs do not directly address pain science but rather teach management of disease from a biomechanical approach”. (3)
More recently, a faculty survey performed by the same authors among accredited physical therapist education programs (Doctorate of Physical Therapy) in the United States reported wide variation in the contact hours devoted to pain content (from 5 to 115 hs, with a mean of 31.8 hs and a mode of 10 hs). Of the 167/216 schools that completed the survey, just 11 (6%) offer an independent course focused on pain; in the vast majority, pain science, assessment, and management are incorporated throughout the curriculum (4)
Are physical therapists optimally prepared to assess, manage, and treat pain? Share on X
Plugging Holes and Filling the Pain Education Gap
This deficit in pain education for physical therapists, however, occurs to various extents across all health professions. For example:
- Only 0.3% of the total curriculum hours for physicians is dedicated to pain science education. A 2011 study in The Journal of Pain found that U.S. medical schools allot a median of 9 teaching hours on pain and its management, compared to a median of 19.5 hours in Canada.
- A 2016 Study in the Journal of Pain Medicine by NIH researcher and pain psychologist Beth Darnall found more than one-quarter of graduate level health psychology coursework do not address pain treatment in the curricula, and…
- Only one-third of psychology programs dedicate 0–4 hours of coursework in pain.
- A 2014 study in the Journal of Advanced Practice Oncology expressed the need for improving pain management at the nursing education level, citing evidence for lack of knowledge as a major hindrance to good pain management practices.

This issue was put forward in 2011 when the NIH’s Department of Health and Human Services requested the Institute of Medicine to convene an interprofessional consensus summit to address the state of the science with respect to pain research, care, and education. The summit’s final report (Relieving Pain in America – A Blueprint for Transforming Prevention, Care, Education, and Research) defined core competencies in pain assessment and management for pre-licensure health professional education (5).
An analysis of the summit’s report written by Marie K. Hoeger Bement,MPT, PhD, Kathleen A. Sluka, PT, PhD and colleagues and published in the journal Physical Therapy highlights that the core competencies would “facilitate the development of a cohesive and comprehensive foundation for educational programs that can be readily shared among health care teams”, and emphasizes their relevance to Physical Therapy programs across the nation (3).
Physical therapists are uniquely positioned to not only effectively treat pain, but to prevent it! Share on XThese competencies, included within four domains, are aligned with the guidelines for pain education curricula published by the International Association for the Study of Pain (IASP) and are summarized below (3):
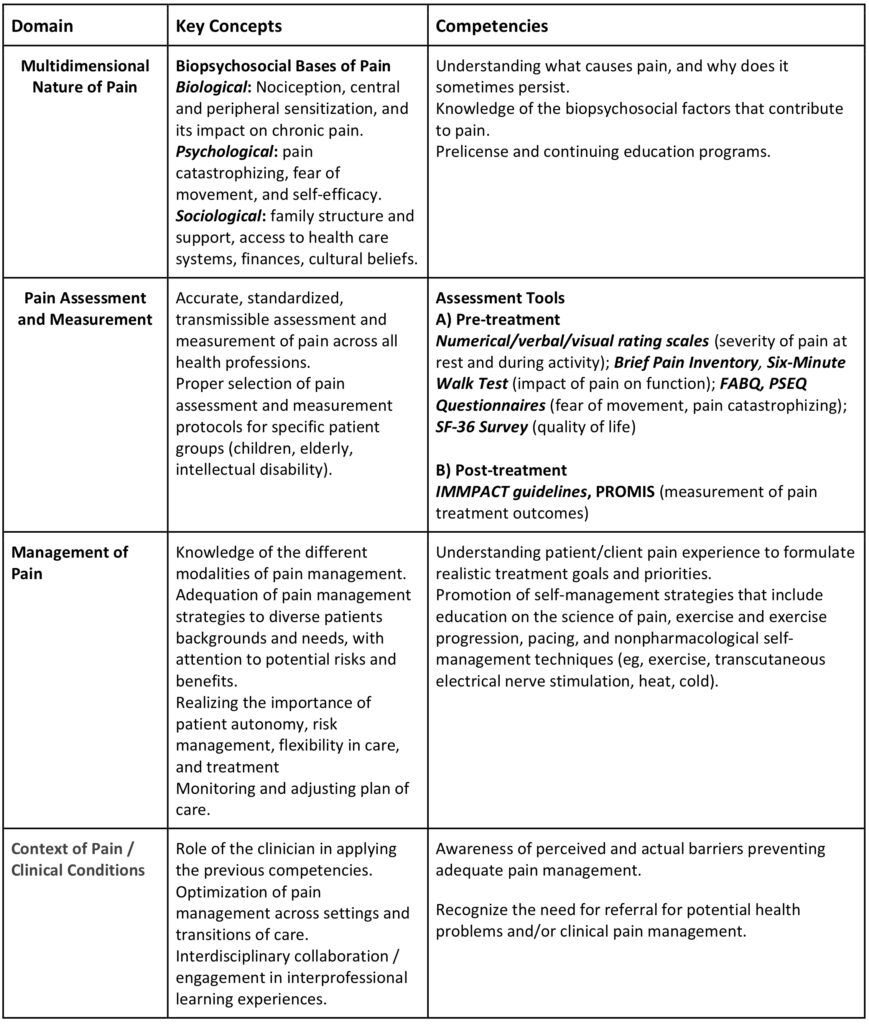
Applying these program competencies into pain education for physical therapists “would ensure that physical therapist students effectively perform and demonstrate skills to reduce pain, improve function and quality of life, and reduce comorbidities and costs related to unrelieved pain.” (3)
Dr. Tatta’s simple and effective pain assessment tools. Quickly and easily assess pain so you can develop actionable solutions in less time.
The Path Ahead: Incorporating Pain Education for Physical Therapists
Drs. Hoeger Bement and Sluka’s article offers several recommendations to effectively incorporate into entry-level Physical Therapy curriculum the pain assessment and management competencies suggested by the interprofessional consensus summit on pain science:
- Addition of a stand-alone pain management course to supplement the integration of pain education throughout the curriculum, emphasizing the science underlying pain, its complex biological and psychosocial effects, its impact on the patient, family, and society, and interprofessional management
- Adherence to the International Classification of Functioning, Disability and Health (ICF) model from the World Health Organization as a foundational educational model
- Integrate pain education for physical therapists by adopting clinical reasoning frameworks for pain assessment and management
- Student engagement in interprofessional learning experiences: courses, seminars, case-based learning activities, etc., that keep up with current pain science research.
Time to Act! Physical Therapy’s Opportunities and Challenges
Formulating an effective pain care program for physical therapists’ patients or clients, and adjusting it as needed during follow-up visits, requires acknowledging the multidimensional nature of pain and how it is perceived by those who experience it; appreciating the diversity, adequacy, benefits and risks of available treatments (pharmacological and natural); the roles that other health professionals play in pain care; and the patient’s expectations, motivations, self-efficacy, and barriers to treatment. Understanding and implementing these core competencies will allow current and future physical therapists to affect profound, long-lasting change in pain treatment and prevention, substantially reducing the human and economic costs that chronic pain brings to the lives of millions of people in America.
We’d love to hear your experience with pain management strategies and education. Please leave us a comment below, and visit us on Facebook!
REFERENCES:
1- American Physical Therapy Association. Vision 2020. Available at: http://www.apta.org/Vision2020/ Accessed September 2018
2- Pendergast J, Kliethermes SA, Freburger JK, Duffy PA. A comparison of health care use for physician-referred and self-referred episodes of outpatient physical therapy. Health Serv Res. 2012;47:633–654
3- Hoeger Bement, M. K., St. Marie, B. J., Nordstrom, T. M., Christensen, N., Mongoven, J. M., Koebner, I. J., … Sluka, K. A. (2014). An Interprofessional Consensus of Core Competencies for Prelicensure Education in Pain Management: Curriculum Application for Physical Therapy. Physical Therapy, 94(4), 451–465.
4- Bement, M. K. H., & Sluka, K. A. (2015). The current state of physical therapy pain curricula in the United States: a faculty survey. The Journal of Pain, 16(2), 144-152.
5- Fishman, S. M., Young, H. M., Lucas Arwood, E., Chou, R., Herr, K., Murinson, B. B., … & Bakerjian, D. (2013). Core competencies for pain management: results of an interprofessional consensus summit. Pain Medicine, 14(7), 971-981.
6- Darnall, B. D., Scheman, J., Davin, S., Burns, J. W., Murphy, J. L., Wilson, A. C., … Mackey, S. C. (2016). Pain Psychology: A Global Needs Assessment and National Call to Action. Pain Medicine (Malden, Mass.), 17(2), 250–263. http://doi.org/10.1093/pm/pnv095



