Pain is an unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage. Nociception and pain are different phenomena. Nociception is the process of encoding noxious stimuli in the nervous system. Pain is a personal experience.
Unrelieved pain is associated with significant disability and socioeconomic burdens. The exorbitant cost of health care and lost productivity associated with pain is approximately $600 billion per year and far exceeds the investment in research to improve the understanding of pain and the development of safe and effective treatments.
In our attempt to understand chronic pain better, it has been categorized according to segments of the body affected or according to different pain mechanisms, including nociceptive, neuropathic or nociplastic. It is widely agreed that chronic pain should be understood as a result of biomedical, psychosocial, contextual behavioral, and epigenetic lifestyle factors. And yet, even with these categories, presumed mechanistic differences, and the recognition of multidimensionality, progress in addressing national and global burden of pain appears slow.
There are many treatments for chronic pain that have helped people around the world. Some are based on scientific evidence that aims to relieve pain, improve mood, or reduce disability. At the same time, pain is a personal experience unique to the individual that impacts health and well-being. No two people experience pain the same way and no two interventions used to target pain plans look the same.
It is suggested that the development of future treatments for chronic pain ought to move away from trying to figure out the one perfect intervention. This is highly unlikely due to the contextual nature of pain. Instead, it has been suggested we adopt a process-based approach that focuses on evidence-based mechanisms of change, unique to the individual, and based on a contextually sensitive assessment.
What is a process-based therapy approach?
A process-based therapy approach is a type of therapeutic method or framework that focuses on the ongoing, dynamic, and evolving nature of a person’s physical, physiological, emotional, and social processes. This approach emphasizes understanding and working with the underlying processes that contribute to a person’s thoughts, feelings, behaviors, health and overall well-being, rather than simply addressing specific symptoms or problems in isolation.
Here are the key characteristics of a process-based therapy:
- Exploration of Current Experience: process-based therapy encourages clients to explore their current experiences, thoughts, and feelings in the present moment. By doing so, clients can gain a deeper understanding of how their internal processes influence their behavior and decision-making.
- Emphasis on Behavior Change: rather than offering direct solutions or advice, process-based therapists facilitate clients’ exploration and self-discovery. Clients are encouraged to identify and understand the underlying processes that contribute to their difficulties. From this place the client can plan their pain recovery.
- The Integration of Different Therapeutic Approaches: process-based therapy is not tied to a single theoretical orientation but can incorporate elements from various therapeutic approaches. The choice of techniques and interventions is guided by what best suits the client’s needs and the evolving therapeutic process.
- Flexible and Adaptable: process-based therapy is highly adaptable to the unique needs and goals of each client. Therapists tailor their approach based on the client’s presenting issues and how the therapeutic process unfolds over time.
- Change is a Natural Outcome: in process-based therapy, change is seen as a natural outcome of increased self-awareness and insight. As clients gain a deeper understanding of themselves and their patterns, they are better equipped to make meaningful changes in their lives.
How to Develop a Process-based Approach to Pain Management
In order to develop a process-based approach to pain management a clinician needs to consider the clinical decision-making process first and identify the essential domains of pain management.
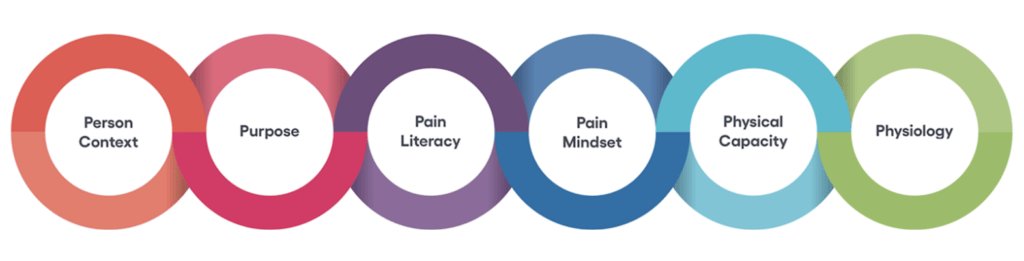
Six domains have been identified that promote pain resilience and facilitate pain recovery. They are:
- Person context
- Purpose
- Pain literacy
- Pain mindset
- Physical capacity
- Physiology
These domains address all four parts of clinical decision-making that have historically been underemphasized in pain care. They are: 1) evidence-informed, 2) identifies patient context as a key domain, 3) considers patient preference for integrative care, and 4) addresses the clinical state through change processes.
A definition of each domain is listed below. These domains address the multidimensional nature of pain, pain assessment; management of pain, and context of pain management. For short we call these the 6 Ps (domains) of Pain Recovery:
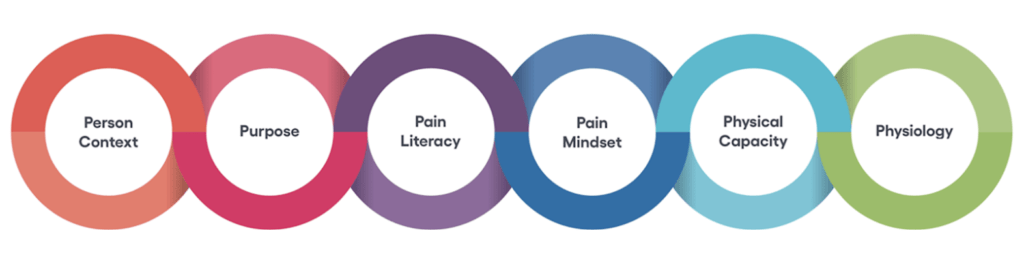
Figure 1: The 6 ‘Ps’ of Pain Recovery
1. Person context: The life circumstances and individual behaviors relevant to planning a particular person’s care
2. Purpose: Forward-looking, generalized intention to accomplish something that is at once meaningful to the self and of consequence to the world beyond the self. It includes an understanding of one’s purpose and direction in life, including goals and beliefs that provide meaning, motivation, and high levels of intention toward pursuing one’s goals.
3. Pain Literacy: Knowledge that enables effective pain self-management. It incorporates a person’s existing knowledge of pain and associated biopsychosocial cultural attitudes and beliefs. Pain literacy is context-specific and focuses on reducing stigma and empowering people with attitudes, beliefs, and behaviors needed to overcome pain.
4. Pain Mindset: There are two types of pain mindsets; fixed and flexible. A flexible mindset is one in which an individual is motivated to change, engages in behaviors that improve mood and pain-related disability and responds flexibly to the lived experience of pain.
5. Physical Capacity: Conceptualized at the person level (rather than impairments in particular body functions or structures), physical capacity encompasses concepts such as strength, range of motion, stamina, balance, proprioception, and load which enable individuals to maintain their functional abilities.
6. Physiology: The functions and activities of life or of living matter (such as organs, tissues, or cells) and of the physical and chemical phenomena involved in pain perception and modulation.
Why Are Process-based Therapies Needed in Pain Care?
Process-based therapies have emerged in response to certain limitations and needs within the field of pain management. There are several reasons why the development of process-based therapies is important.
First, process-based therapies recognize that the human experience of pain is complex and multifaceted. They seek to address issues at a deeper level by exploring the underlying processes, emotions, and patterns that contribute to a client’s difficulties. This holistic approach allows for a more comprehensive understanding of clients’ lives and issues. Next, people are unique, and their experiences and challenges are often highly individualized. Process-based therapies prioritize tailoring the therapeutic approach to the specific needs and goals of each client. This individualization increases the likelihood of successful outcomes in therapy. They also consider that human beings are constantly evolving and changing. Process-based therapies acknowledge that personal growth and healing are ongoing processes, and they help clients navigate these changes. This is particularly important for clients dealing with issues that may not have clear, static solutions. With this, there is an emphasis on self-awareness. Process-based therapies place a strong emphasis on self-awareness and mindfulness. They help clients develop a deeper understanding of themselves, their thought patterns, emotions, and behaviors. This self-awareness is often a crucial foundation for making positive changes in one’s life. The therapeutic relationship is a central component of process-based therapy. Research has consistently shown that the quality of the therapeutic relationship strongly influences treatment outcomes. By focusing on the dynamics of this relationship, process-based therapies aim to enhance its effectiveness.
Process-based therapies are also known to be flexible and integrate techniques from various therapeutic approaches. This adaptability allows therapists to draw from a wide range of tools and strategies to meet clients where they are and address their unique needs. There is also a depth of insight. Process-based therapies aim to help clients achieve a deep level of insight into their thoughts, emotions, and behaviors. This deeper understanding often leads to lasting changes and improved psychological well-being. This is critical because many clients come to therapy with complex and layered issues, such as trauma or longstanding difficulties. Process-based therapies are well-suited to working with these complex challenges by delving into the underlying dynamics and patterns that contribute to these issues. Finally, process-based therapies are flexible and responsive. The dynamic nature of process-based therapies allows therapists to adapt their approach as the therapeutic process unfolds. This responsiveness to the client’s evolving needs and insights can be especially beneficial.
Conclusion
Future treatments for chronic pain should incorporate process-based approaches, focused on evidence-based mechanisms of change, that consider the individual, and are individually contextually sensitive. Empirically supported biopsychosocial processes of change known to be functionally important should be identified in pain management. The long list of change processes in pain management necessitates the selection of appropriate priorities to develop, evaluate, and implement. A well-designed model of pain care goes beyond risk factor identification to encompass mediators and moderators of change, as well as biomedical, psychosocial, contextual behavioral, and epigenetic lifestyle factors.
In summary, process-based therapies are developed to provide a more comprehensive, individualized, and flexible approach to therapy. They recognize the complexity of human experience and aim to help clients achieve meaningful and lasting change by exploring and addressing the underlying processes that contribute to their issues. In the next blog, I will address specific processes of change known to impact pain and lead to pain recovery.
Joe Tatta, PT, DPT
CEO Integrative Pain Science Institute
Learn more at integrativepainscienceinstitute.com or join our mailing list here!
Main Reference:
Tatta J, Pignataro RM, Bezner JR, George SZ, Rothschild CE. PRISM – Pain Recovery and Integrative Systems Model: A Process-Based Cognitive-Behavioral Approach for Physical Therapy [published online ahead of print, 2023 Jun 27]. Phys Ther. 2023;pzad077. doi:10.1093/ptj/pzad077
Supporting References
Hofmann SG, Hayes SC. The Future of Intervention Science: Process-Based Therapy. Clin Psychol Sci. 2019;7(1):37-50. doi:10.1177/2167702618772296
McCracken LM. Personalized pain management: Is it time for process-based therapy for particular people with chronic pain?. Eur J Pain. 2023;27(9):1044-1055. doi:10.1002/ejp.2091
Åkerblom, S., Perrin, S., Rivano Fischer, M., & McCracken, L. M. (2021). Predictors and mediators of outcome in cognitive behavioral therapy for chronic pain: The contributions of psychological flexibility. Journal of Behavioral Medicine, 44(1), 111-122. https://doi.org/10.1007/s10865-020-00168-9



