Cognitive-behavioral therapy (CBT) has shown to be highly effective in fields outside of traditional psychotherapy. Research illustrating the benefit of CBT techniques for patients with persistent pain has led physical therapists to explore their use. (1) Have you currently incorporated cognitive-behavioral skills into your clinical practice? The following is a 7-step framework for integrating CBT skills into the treatment plan of a patient with persistent lower back pain (LBP) and can be applied to many chronic pain syndromes.
Seven Types of Cognitive-Behavioral Skill
1. Activity Pacing
Chronic pain patients often associate movement with pain, leading to the unfortunate avoidance of activities altogether. Activity Pacing enables the patient to re-establish a healthy relationship to movement by gradually exposing them to daily functional activity and increasing the intensity or exposure. The objective is to help the client establish “consistent, moderate engagement in physical, recreational, and social activities.” (2) A therapist can encourage a client with low back pain to take breaks at work, establish a consistent pace, manage tasks more appropriately, or reduce the speed of their activity.

2. Attention Diversion
The objective here is to divert the client’s attention away from pain and its associated stress and towards the use of enjoyable goal-oriented activities. A therapist might encourage a patient with low back pain to return to previously enjoyed hobbies or pastimes, such as shopping, golfing, group exercise classes, weight training, childcare in alignment with the activity-pacing principles.
3. Cognitive Restructuring
This is key to successfully implementing CBT skills into a clinical practice. Identifying and helping to modify maladaptive beliefs, thoughts, or emotions is paramount. For example, once ‘fear-avoidance’ is identified, a more comprehensive treatment program can be designed. If a client with chronic LBP associates pain with taking long walks, a walking schedule using graded exposure might help to dissolve the fear associated with movement. Educating patients on the normalcy of flare-ups—eliminating the fear that flare-ups signal a worsening condition—can go far in reducing patient anxiety. Cognitive restructuring to change the patient’s perception of pain avoidance can be targeted with pain physiology education such as those based on Explain Pain by Butler and Moseley. Verbal reinforcement emphasizing that pain does not necessarily correlate with tissue damage and the encouragement to maintain a consistent, gradually progressive exercise program irrespective of pain level is the goal. Cognitive restructuring and pain education has been shown to improve pain attitudes, pain catastrophizing, and physical performance.
4. Goal Setting
In a study of adults with chronic pain, goal-setting correlated to goal attainment, which isn’t surprising! (3) Tangibly tracking self-efficiency via an exercise notebook, or a progress log that records adherence to a home exercise program, can positively influence a patient’s sense of personal achievement. (4) Goals for patients with low back pain might include increased walking time, weight loss, or higher tolerance to sitting at work.

5. Graded Exposure
Graded exposure refers to the systematic progression of a client’s exercise from their baseline level of tolerability. Exposing your patient to increased physical “stress” at a reasonable rate has been shown to reduce pain catastrophizing and perceived harmfulness of activities in subjects with chronic low back pain. (4, 5) A walking program that utilizes an exercise log, designed to encourage incremental increases over time is an excellent and common example.
Exposing your patient to increased physical “stress” at a reasonable rate has been shown to reduce pain catastrophizing Share on X6. Maintenance Strategies
Patients can be taught strategies, such as ways to handle flare-ups and means of addressing future pain episodes. Physical therapists will also want to follow up on patient adherence to their treatment plan and adjust the program as needed. Maintenance includes activity progression and skills education. Of key importance is emphasizing to the patient the purpose of their home program and the value of maintaining movements and activities within their pain parameters.
Dr. Tatta’s simple and effective pain assessment tools. Quickly and easily assess pain so you can develop actionable solutions in less time.
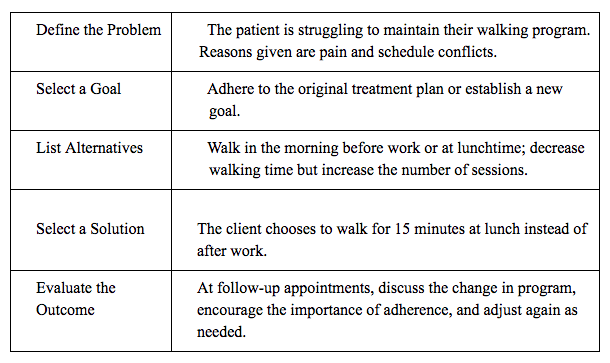
7. Problem-Solving Strategies
Problem-solving has been defined as a multi-step process that includes: (6)
- Define the problem
- Select a goal
- List alternatives
- Select a solution
- Evaluate the outcome and adjust as needed
The following table summarizes how to implement a problem-solving strategy for a patient with lower back pain:
The effectiveness of CBT in managing chronic pain is growing and multiple examples of physical therapists applying CBT principles in practice are spreading. Having knowledge of cognitive-behavioral therapy tools and techniques enhances the skills of other health care practitioners, including physiotherapists, and that adding these to one’s skill repertoire can improve patient outcomes. Still, the use of CBT techniques is underutilized by physical therapists in treating chronic pain. Incorporated CBT techniques into existing patient education efforts by physical therapists is a valuable step in helping improve outcomes when managing patients with chronic pain.
Are you interested in learning more about the relation between cognition and pain? Have you already begun to integrate these skills into your practice? Find us on Facebook! We’d love to hear from you.
REFERENCES:
- Eccleston C, Williams AC, Morley S. Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst Rev2009;CD007407.
- Murphy JL, McKellar JD, Raffa SD, et al. Cognitive behavioral therapy for chronic pain among veterans: therapist manual. Washington (DC): U.S. Department of Veterans Affairs.
- Davis GC, White TL. A goal attainment pain management program for older adults with arthritis. Pain Manag Nurs 2008;9:171-9.
- Rundell SD, Davenport TE. Patient education based on principles of cognitive behavioral therapy for a patient with persistent low back pain: a case report. Journal of Orthopaedic and Sports Physical Therapy 2010;40:494-501.
- Leeuw M, Goossens ME, van Breukelen GJ, et al. Exposure in vivo versus operant graded activity in chronic low back pain patients: results of a randomized controlled trial. Pain 2008;138:192-207.
- Turk DC. Clinical effectiveness and cost-effectiveness of treatments for patients with chronic pain. Clin J Pain 2002;18:355-65.